Gut health has become a major topic of interest for medical professionals, nutritionists, and wellness enthusiasts alike. For a long time, the digestive system was considered merely responsible for breaking down food and extracting nutrients. However, modern research has revealed that our gastrointestinal tract plays a pivotal role in our immune function, mental well-being, and overall vitality. From producing essential vitamins to communicating with your brain through the gut-brain axis, your digestive system does a lot more than just process what you eat.
Your gut microbiome—the ecosystem of microbes living in your intestines—impacts almost every aspect of health: mood regulation, weight management, immune response, inflammation levels, and nutrient absorption. Imbalances in this microbiome can manifest in problems like bloating, constipation, diarrhea, fatigue, and even mental health conditions like anxiety and depression.
In this comprehensive article, we’ll delve deep into the fundamentals of gut health, explain how digestion works, identify common digestive issues, and discuss both dietary and lifestyle changes you can make to improve your microbiome. By the end, you’ll be equipped with evidence-based insights and practical tips to nurture a healthier, happier gut.
Table of Contents
What Is the Gut Microbiome?

The term “gut microbiome” refers to the community of microorganisms—bacteria, fungi, viruses, and other microbes—that live predominantly in the large intestine (colon) but also throughout the digestive tract. These microorganisms are critical for many bodily functions, helping to break down certain food components, produce vitamins, and protect against harmful pathogens.
Composition of the Microbiome
Your gut microbiome is extraordinarily diverse, housing trillions of microbes of hundreds of different species. While we often focus on bacteria, the microbiome also includes smaller numbers of yeasts, viruses, and protozoa. Some of the most well-known bacterial genera in the human gut include Bacteroides, Lactobacillus, Bifidobacterium, and Ruminococcus.
Key points regarding microbiome composition:
- The diversity of bacterial species can vary significantly from person to person.
- The composition is influenced by genetics, diet, lifestyle, and even geography.
- Microbial diversity is often considered a marker of good gut health.
Beneficial vs Harmful Bacteria
While we often fear the word “bacteria,” it’s important to recognize that many bacterial strains are beneficial or even essential for our well-being. The beneficial strains help with tasks such as:
- Synthesizing vitamins: Some gut bacteria produce vitamins like vitamin K and certain B vitamins.
- Protecting the gut lining: By maintaining the mucosal layer, helpful bacteria prevent pathogens from entering the bloodstream.
- Supporting immunity: Beneficial microbes stimulate immune cells, helping the body fight infections.
On the other hand, certain harmful or pathogenic bacteria (e.g., Clostridium difficile or certain strains of E. coli) can cause infections or contribute to conditions like diarrhea and inflammation. The delicate balance between these helpful and harmful bacteria is essential for robust gut health.
Factors Influencing Your Microbiome
Numerous factors can alter the composition and function of your microbiome, including:
- Diet: The types of foods you consume—high-fiber foods, fermented foods, processed sugars—can significantly impact bacterial diversity.
- Antibiotics and Medications: Antibiotics, while often necessary, can disrupt the microbial balance by killing both harmful and beneficial bacteria.
- Stress: Chronic stress can decrease the diversity of your gut flora and increase harmful bacteria.
- Sleep: Irregular sleep patterns and poor sleep quality can disrupt gut bacteria balance.
- Age: As you age, the composition of your microbiome shifts, often becoming less diverse.
Understanding these factors sets the stage for making informed choices that foster a healthy and diverse gut microbiome.
How Digestion Works
Digestion is the complex process of turning the food you eat into the nutrients your body needs to function properly. This process involves multiple organs and systems, from the mouth and stomach to the intestines and liver. Each step is orchestrated through a combination of muscular contractions, enzyme actions, and gut microbes.
Key Stages of Digestion
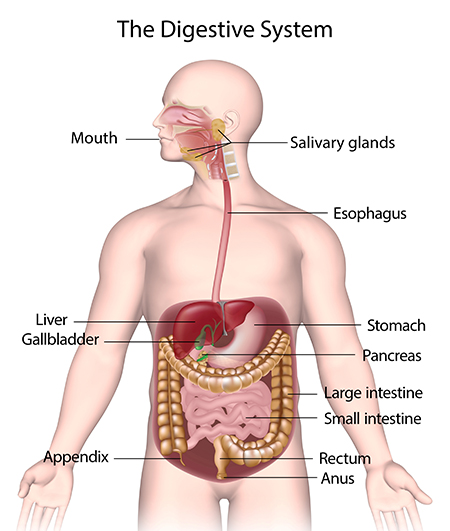
- Mouth: Digestion starts the moment you begin chewing. Saliva contains enzymes like amylase, which starts breaking down carbohydrates.
- Esophagus: A muscular tube that transports food from your mouth to your stomach through rhythmic contractions called peristalsis.
- Stomach: Here, acids and enzymes break down food, particularly proteins. The stomach’s acidic environment also helps kill many pathogens.
- Small Intestine: The majority of nutrient absorption occurs here. Bile from the gallbladder and enzymes from the pancreas aid in breaking down fats, carbohydrates, and proteins.
- Large Intestine (Colon): This is where most of the microbiome resides. Water and electrolytes are reabsorbed here, and undigested food (especially fiber) is fermented by gut bacteria.
- Rectum and Anus: Finally, waste products are expelled from the body through the rectum and anus.
The Role of Digestive Enzymes
Digestive enzymes are specialized proteins that help break down macronutrients into smaller, more easily absorbed molecules. Key enzymes include:
- Proteases (e.g., pepsin, trypsin) for breaking down proteins into amino acids.
- Amylases (in saliva and pancreatic secretions) for breaking down carbohydrates into simple sugars.
- Lipases (primarily from the pancreas) for digesting fats into fatty acids and glycerol.
Enzyme deficiency or insufficiency can lead to bloating, gas, and malabsorption of nutrients. Certain health conditions (like chronic pancreatitis or cystic fibrosis) can compromise enzyme production, but even subclinical enzyme deficiencies can affect digestion and gut health.
How Gut Bacteria Impact Digestion
Beyond enzymes, your gut bacteria play a huge role in digestion. These microorganisms ferment dietary fiber and certain starches, producing short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. SCFAs serve multiple functions:
- Nourishing colon cells: SCFAs provide energy to the cells lining your colon, keeping them healthy and reducing inflammation.
- Regulating appetite and metabolism: Some SCFAs can influence hormones involved in appetite control, such as leptin and ghrelin.
- Enhancing mineral absorption: Gut bacteria can help increase the absorption of minerals like calcium and magnesium.
A balanced microbiome synergizes with your digestive enzymes, ensuring nutrients are effectively extracted and waste is promptly eliminated.
Common Digestive Issues and Their Causes

While occasional digestive discomfort is normal, recurring symptoms may indicate an underlying gut imbalance or health condition. Understanding common digestive problems can help you identify potential triggers and seek targeted solutions.
1. Irritable Bowel Syndrome (IBS)
IBS is a functional gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits (diarrhea, constipation, or both). While the exact cause is not fully understood, factors may include:
- Gut hypersensitivity: An overly sensitive gut that reacts strongly to normal stimuli.
- Imbalanced microbiome: Reduced bacterial diversity, an overgrowth of certain bacteria, or low levels of beneficial bacteria.
- Gut-brain axis dysfunction: Stress and mental health challenges can exacerbate IBS symptoms.
2. Gastroesophageal Reflux Disease (GERD)
GERD involves chronic acid reflux, where stomach acid frequently flows back into the esophagus, causing heartburn and irritation. This can be triggered by:
- A weak lower esophageal sphincter (LES): This valve-like muscle fails to close properly, allowing acid to escape.
- Dietary choices: Spicy foods, citrus, chocolate, caffeine, and alcohol can worsen reflux.
- Obesity: Excess abdominal fat can increase pressure on the stomach.
3. Leaky Gut Syndrome
Leaky gut refers to increased intestinal permeability, where gaps in the intestinal lining allow larger molecules (like toxins and partially digested food particles) to pass into the bloodstream. This can trigger inflammatory responses and has been linked to autoimmune diseases. Contributing factors may include:
- Chronic inflammation
- Poor diet (especially high in sugar and processed foods)
- Excessive alcohol consumption
- Overuse of medications (like NSAIDs and antibiotics)
4. Small Intestinal Bacterial Overgrowth (SIBO)
SIBO occurs when bacteria that typically reside in the large intestine overgrow in the small intestine. This can lead to:
- Nutrient malabsorption
- Gas and bloating
- Diarrhea or constipation
Factors like low stomach acid, slow gut motility, and structural abnormalities can predispose someone to SIBO.
5. Chronic Inflammation and Autoimmune Conditions
Imbalanced gut flora is often associated with systemic inflammation, which can contribute to autoimmune conditions such as Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and more. While genetic predisposition is often a factor, environmental triggers like diet and lifestyle can fuel or soothe the inflammatory process.
The Gut-Brain Axis: How Your Gut Affects Your Mind

One of the most fascinating discoveries of modern science is the gut-brain axis—the bidirectional communication network linking your enteric nervous system (the “second brain” in your gut) with your central nervous system. This relationship is mediated by the vagus nerve, hormones, and neurotransmitters like serotonin and dopamine.
- Serotonin Production: About 90% of your body’s serotonin—a neurotransmitter linked to mood regulation—is produced in the gut.
- Stress Response: Chronic stress can negatively impact the gut lining, reduce beneficial microbes, and increase harmful bacterial strains.
- Mental Health: Imbalances in gut flora have been linked to anxiety, depression, and even neurodegenerative conditions like Parkinson’s disease.
Understanding the gut-brain axis highlights the importance of nurturing your gut not just for physical well-being, but also for emotional and mental health.
Foods for a Healthy Gut

Improving gut health starts with the foods you choose to put on your plate. A balanced diet rich in fiber, fermented foods, and whole, unprocessed ingredients can foster a more diverse and robust microbiome.
Prebiotics, Probiotics, and Synbiotics
- Prebiotics: These are non-digestible fibers that fuel the growth of beneficial gut bacteria. Examples include inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS). You can find them in foods like onions, garlic, asparagus, and chicory root.
- Probiotics: These are live microorganisms that confer health benefits. Common strains include Lactobacillus and Bifidobacterium, found in foods like yogurt, kefir, and certain supplements.
- Synbiotics: A combination of both prebiotics and probiotics, designed to support the survival and colonization of probiotic strains in the gut.
Fermented Foods
Fermented foods are a potent source of natural probiotics. Incorporating these can help restore or maintain a healthy microbial balance. Examples include:
- Yogurt (preferably unsweetened)
- Kefir
- Sauerkraut
- Kimchi
- Kombucha
- Miso
When adding fermented foods to your diet, start slowly, especially if you’re new to them. Some people experience temporary bloating or gas as their gut adjusts.
Dietary Fiber
Fiber is crucial for maintaining healthy bowel movements and fueling beneficial gut bacteria. There are two main categories of dietary fiber:
- Soluble fiber: Dissolves in water and forms a gel-like substance, helping to regulate blood sugar and cholesterol. Found in oats, beans, fruits, and flaxseeds.
- Insoluble fiber: Does not dissolve in water and adds bulk to stool, promoting regularity. Found in whole grains, nuts, and many vegetables.
Aim for a variety of fiber sources to feed a broad spectrum of gut microbes. Gradually increase your fiber intake to avoid excessive gas or bloating.
Whole Foods vs Processed Foods
A diet rich in whole foods (vegetables, fruits, nuts, seeds, legumes, and lean proteins) nourishes a diverse microbial environment. Conversely, diets high in processed foods, refined sugars, and artificial additives can diminish microbial diversity and increase inflammation.
Example Meal Plan for Gut Health
- Breakfast: Oatmeal topped with berries, chia seeds, and a dollop of plain yogurt for probiotics.
- Lunch: Mixed greens salad with grilled chicken, quinoa, roasted vegetables, and a drizzle of olive oil and lemon juice.
- Snack: Apple slices with almond butter (prebiotic fiber and healthy fats).
- Dinner: Salmon with a side of steamed asparagus, and a serving of sauerkraut or kimchi.
Lifestyle Factors That Influence Gut Health

While diet is integral, other lifestyle components also significantly shape your microbiome. Addressing these factors is often the missing piece in long-term gut health strategies.
Stress and Gut Health
Chronic stress can alter gut motility, reduce beneficial bacteria, and even increase intestinal permeability. High-stress levels may worsen symptoms in IBS, GERD, and other gut disorders. Techniques like mindfulness meditation, yoga, journaling, or therapy can reduce stress and improve gut health over time.
Physical Activity and Movement
Regular exercise promotes efficient digestion, supports a balanced microbiome, and helps manage stress. Low-impact activities like walking, swimming, or cycling can be especially beneficial for those with sensitive digestive systems. Even 30 minutes of moderate exercise a day can yield noticeable improvements in gut function.
Sleep and Circadian Rhythm
Sleep is a critical regulator of many bodily functions, including the gut microbiome. Poor sleep quality or disrupted sleep patterns can negatively affect microbial balance and increase inflammation. Aim for 7–9 hours of quality sleep per night, and try to maintain a consistent sleep schedule (going to bed and waking up at roughly the same time each day).
Hydration
Staying adequately hydrated aids digestion, helps transport nutrients, and supports regular bowel movements. Aim for at least 8 cups (64 ounces) of water per day, though individual needs may vary depending on factors like activity level, climate, and overall health.
Signs of an Unhealthy Gut
Recognizing the warning signs of a gut in distress can help you take corrective action sooner rather than later. Some common indicators include:
- Frequent Bloating and Gas: Excessive fermentation by bacteria, often due to imbalances in the gut microbiome or certain food intolerances.
- Irregular Bowel Movements: Chronic constipation or diarrhea could be a sign of underlying issues like IBS, SIBO, or inadequate fiber intake.
- Food Intolerances or Sensitivities: If you notice symptoms like bloating, cramps, or fatigue after eating certain foods, you may have an intolerance or leaky gut issues.
- Fatigue and Low Energy: Poor nutrient absorption can lead to low energy levels and even contribute to conditions like anemia.
- Skin Problems: Acne, eczema, and other inflammatory skin conditions are sometimes linked to poor gut health.
- Frequent Illnesses: Since much of the immune system resides in the gut, an unhealthy gut can compromise immune response.
If you’re experiencing any combination of these symptoms regularly, consider seeking a healthcare professional’s guidance and focusing on gut-supportive lifestyle and dietary changes.
Supplements and Supportive Therapies
While a balanced diet and healthy lifestyle should be the foundation, supplements can offer additional support for those dealing with persistent gut imbalances or specific nutritional deficiencies.
Probiotic Supplements
Probiotic supplements come in various strains and formulations, each targeting different health concerns. When choosing a probiotic, consider:
- CFU (Colony Forming Units): Aim for a product with at least 1 billion CFU per serving (some formulas offer up to 50 billion or more).
- Specific Strains: Different bacterial strains (e.g., Lactobacillus acidophilus, Bifidobacterium longum) can address specific issues like IBS, diarrhea, or immune support.
- Storage and Shelf Life: Some probiotics require refrigeration to maintain potency, while others are shelf-stable.
Digestive Enzymes
Digestive enzyme supplements can help people who struggle with bloating, gas, or indigestion, especially after protein-heavy or fatty meals. Common enzyme supplements contain:
- Proteases for proteins
- Lipases for fats
- Amylases for carbohydrates
- Lactase for lactose breakdown
It’s essential to talk to a healthcare provider before starting an enzyme supplement, to tailor the formulation to your specific needs.
Herbal Teas and Natural Remedies
Herbal teas like peppermint, ginger, and chamomile can soothe digestive discomfort and support a healthy gut environment. Additionally, aloe vera juice and slippery elm are sometimes used to reduce inflammation and protect the intestinal lining. Remember that these remedies should complement, not replace, professional medical advice.
Vitamins and Minerals
Certain nutrients are particularly crucial for maintaining a strong gut lining and robust immunity:
- Vitamin D: Supports immune function and modulates inflammation.
- Zinc: Essential for tissue repair, including the gut lining.
- Magnesium: Assists with muscle relaxation and regular bowel movements.
If you suspect deficiencies, a simple blood test can help identify which vitamins or minerals you should target.
Long-Term Strategies for Optimal Gut Health

Achieving and maintaining a healthy microbiome is a marathon, not a sprint. Here are long-term strategies to keep your gut in optimal shape:
- Variety in Diet: Rotate different types of proteins, whole grains, fruits, and vegetables to feed a wide range of bacterial species.
- Mindful Eating: Chew thoroughly, eat slowly, and listen to hunger and fullness cues to reduce overeating and improve digestion.
- Periodic Evaluations: If you have a chronic condition, consider periodic stool tests or microbiome analyses to monitor shifts in bacterial communities.
- Personalized Approach: Everyone’s microbiome is unique. What works for one person may not work for another, so be open to adjusting your diet and lifestyle.
- Stress Management: Incorporate daily stress-relief practices like breathing exercises, yoga, or mindfulness.
- Stay Active: Regular exercise can positively influence gut flora diversity.
- Limit Antibiotic Use: Only use antibiotics when medically necessary and consider probiotics after a course of antibiotics to help restore beneficial bacteria.
- Cut Down on Sugar and Processed Foods: High sugar intake can fuel harmful bacteria and yeast overgrowth.
Putting It All Together
To achieve a healthier gut, focus on holistic changes rather than quick fixes. Start by evaluating your current diet, gradually introducing more fiber, fermented foods, and nutrient-dense ingredients. Pair dietary adjustments with improvements in sleep, stress management, and physical activity. If symptoms persist, seek professional help to identify underlying conditions and consider targeted therapies like probiotics or enzyme supplements.
Below is a concise checklist to guide you:
- Assess Current Eating Habits
- Are you consuming enough fiber?
- Do you eat fermented foods regularly?
- Are you avoiding excessive processed foods and sugars?
- Lifestyle Audit
- How many hours do you sleep?
- Do you engage in stress-reduction activities?
- Are you physically active most days of the week?
- Monitor Symptoms and Adjust
- Keep a food journal to track reactions to new foods.
- Note any mood changes, energy shifts, or sleep disturbances alongside dietary changes.
- Consider Professional Guidance
- Nutritional consultations, gastroenterologists, and functional medicine practitioners can offer personalized insights.
Frequently Asked Questions (FAQ)
1. How do I know if my gut is healthy?
A healthy gut is often reflected in regular, pain-free bowel movements, minimal bloating or gas, and sustained energy levels. Other indicators include clear skin, a robust immune system, and stable mood. If you frequently experience digestive discomfort, fatigue, or skin issues, it could signal an imbalance.
2. Should I take probiotic supplements every day?
Probiotic needs vary from person to person. Some individuals benefit from daily supplementation—particularly if they’ve recently taken antibiotics or have chronic gut issues—while others may get enough beneficial bacteria from their diet (e.g., fermented foods like yogurt or kimchi). It’s best to consult a healthcare professional to determine the right approach for you.
3. Can stress really affect my digestion?
Yes. Chronic stress can alter gut motility, reduce beneficial bacteria, and even increase intestinal permeability (“leaky gut”). Practicing stress management techniques such as meditation, yoga, or regular exercise can help restore balance to both your mind and your gut.
4. What’s the easiest way to add more fiber to my diet?
Start by incorporating more whole, plant-based foods. Swap refined grains for whole grains like oatmeal, brown rice, or quinoa. Include beans, lentils, and plenty of vegetables in your meals. Gradually increasing your fiber intake helps avoid excessive gas or bloating.
5. When should I see a doctor about gut issues?
If you experience persistent symptoms such as severe abdominal pain, chronic diarrhea or constipation, unexplained weight loss, or signs of malnutrition, seek medical advice. A healthcare professional can perform the necessary tests to rule out conditions like IBS, inflammatory bowel disease, or food intolerances.
Conclusion
Gut health is a fundamental pillar of overall well-being, influencing everything from immune function and nutrient absorption to mental clarity and emotional balance. By understanding the microbiome, honing in on digestive processes, recognizing common gut issues, and implementing dietary and lifestyle strategies, you can profoundly impact your quality of life.
A healthy gut doesn’t happen overnight—it’s a continuous journey that involves nourishing yourself with diverse, whole foods, staying active, managing stress, and getting enough sleep. Whether you’re dealing with a chronic digestive condition or simply looking to optimize your health, these strategies can help you cultivate a more resilient gut and a more vibrant life.
Remember: Always consult with healthcare professionals for personalized advice, especially if you’re experiencing severe or persistent digestive issues. Your gut health is an investment in your long-term wellness, and every step you take toward balancing your microbiome will pay dividends for your body and mind for years to come.