Maintaining optimal thyroid function is critical for a woman’s overall health. Your thyroid influences everything from metabolic rate and energy levels to menstrual cycles and fertility. Unfortunately, many women go undiagnosed or are under-treated for thyroid imbalances for years, leading to a host of health complications. This comprehensive article explores the importance of the thyroid in women’s health, the role of iodine, herbal support for thyroid care, and a detailed symptom checker to help you stay informed.
We will delve into the basics of thyroid physiology, common thyroid disorders affecting women, and how to work with natural remedies like iodine and herbal support. We will also share practical tips on testing, diagnosis, and self-monitoring to keep your thyroid functioning optimally. By the end of this guide, you will have a thorough understanding of women’s thyroid care, backed by research and best practices.
Table of Contents
Understanding the Thyroid Gland
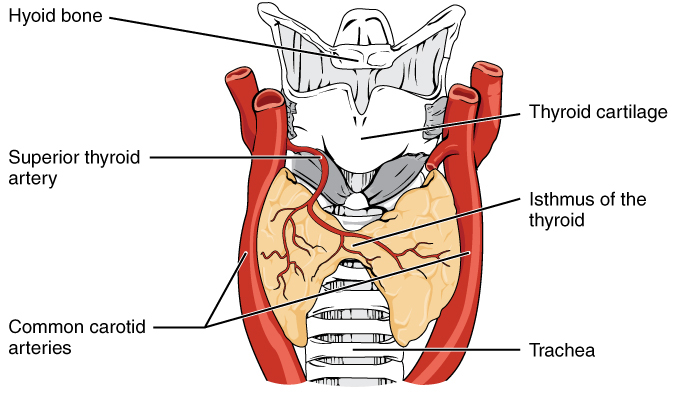
What is the Thyroid?
The thyroid is a small, butterfly-shaped gland located at the front of your neck, just below the Adam’s apple. Despite its modest size, the thyroid plays an outsize role in regulating various physiological functions through the hormones it produces. In particular, the thyroid secretes two primary hormones: thyroxine (T4) and triiodothyronine (T3). These hormones orchestrate metabolic processes, impacting how your body uses energy.
Thyroid function is regulated by a feedback loop involving the hypothalamus, pituitary gland, and the thyroid gland itself:
- The hypothalamus in the brain secretes Thyrotropin-Releasing Hormone (TRH).
- TRH prompts the pituitary gland to release Thyroid Stimulating Hormone (TSH).
- TSH signals the thyroid to produce and release T4 and T3.
This hormonal interplay ensures the body maintains adequate levels of thyroid hormones for optimal health.
Thyroid Hormones: T4, T3, TSH, and More
- T4 (Thyroxine): The thyroid primarily produces T4, which can be converted into the more biologically active T3 in various tissues throughout the body, including the liver and kidneys.
- T3 (Triiodothyronine): Although less abundant, T3 is more potent and has a more profound effect on the body’s metabolic processes.
- TSH (Thyroid Stimulating Hormone): This hormone, released by the pituitary gland, is a critical indicator used in blood tests to assess thyroid function. Elevated TSH often signals an underactive thyroid (hypothyroidism), while low TSH can signify hyperthyroidism or overactive thyroid function.
- Reverse T3 (rT3): A biologically inactive form of T3 that can compete with regular T3 at cellular binding sites. High levels of reverse T3 can inhibit optimal thyroid function.
Why Thyroid Health Matters for Women
Women are far more likely than men to develop thyroid disorders due to complex hormonal interplay involving estrogen, progesterone, and other female hormones. Key life stages—such as puberty, pregnancy, postpartum, and perimenopause—can trigger shifts in thyroid hormone requirements. For instance, pregnancy demands higher thyroid hormone levels to support both maternal and fetal development. Postpartum hormonal changes can also stress the thyroid, leading to transient or long-term thyroid imbalances.
In addition to reproductive factors, autoimmune conditions such as Hashimoto’s thyroiditis or Graves’ disease are more prevalent in women, likely due to female immune system patterns. Untreated thyroid issues can negatively affect fertility, pregnancy outcomes, weight management, mood, and energy levels—underscoring the critical need for proactive thyroid care at every life stage.
Common Thyroid Disorders in Women
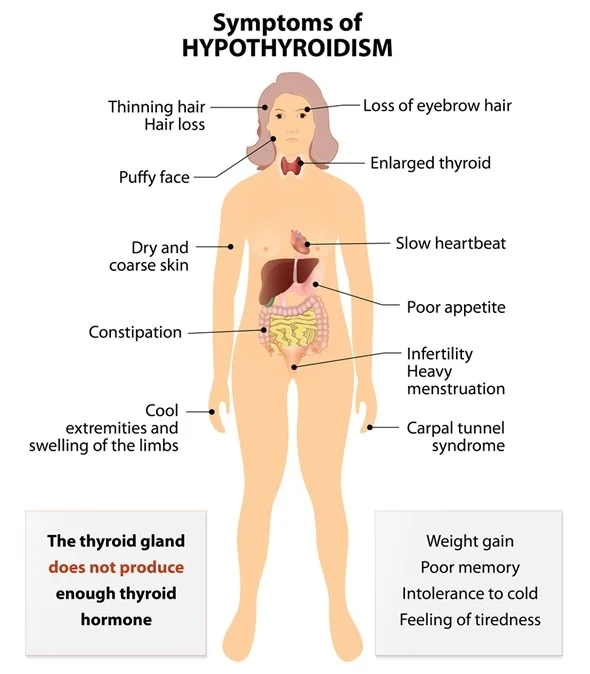
Hypothyroidism (Underactive Thyroid)
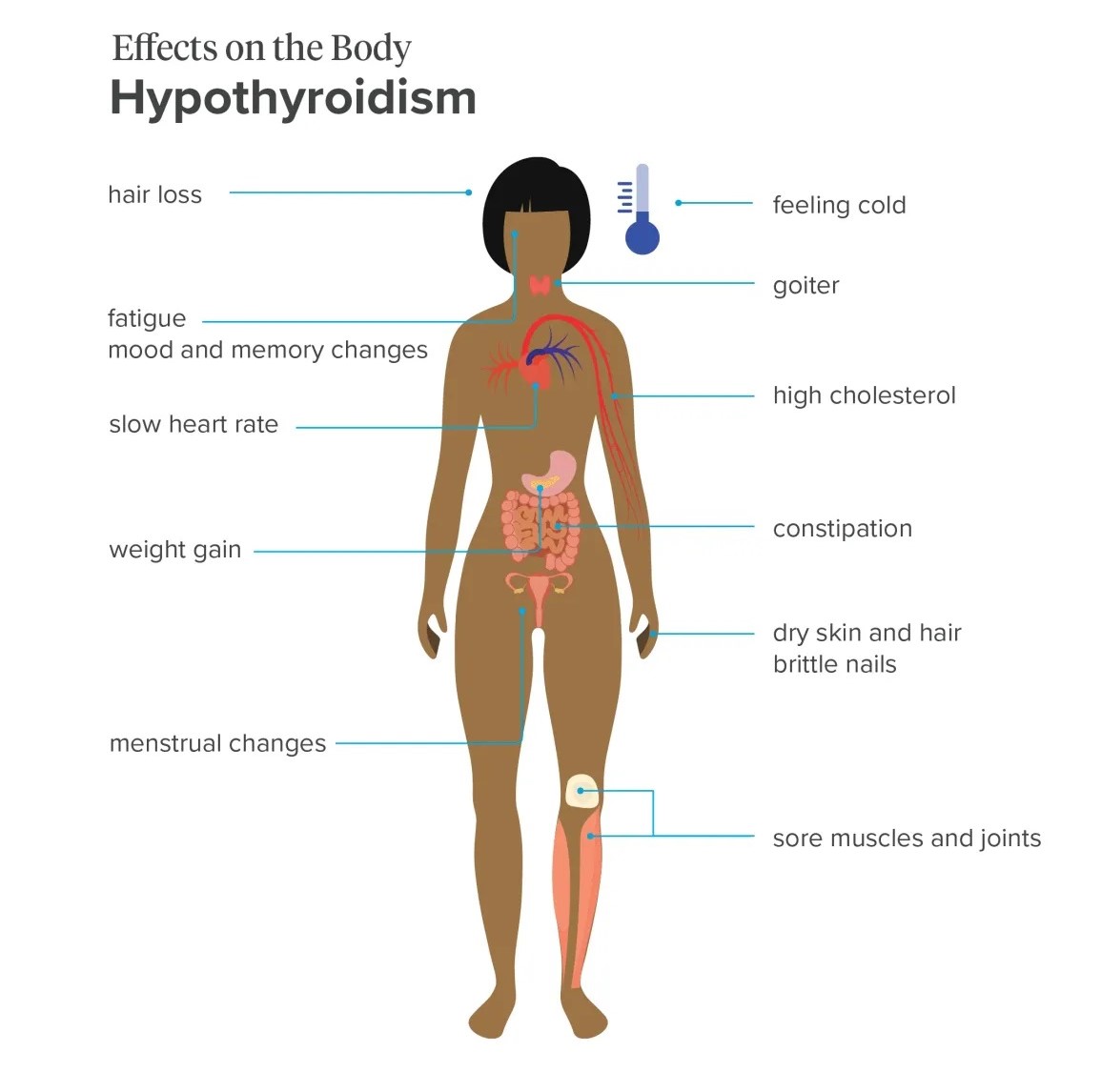
Hypothyroidism is characterized by insufficient thyroid hormone production. When the thyroid gland cannot produce adequate amounts of T4 and T3, bodily functions slow down. Symptoms often appear gradually and can sometimes be mistaken for normal aging or overlooked entirely.
Common symptoms include:
- Persistent fatigue
- Weight gain or difficulty losing weight
- Cold intolerance
- Dry skin, brittle hair, and nails
- Constipation
- Menstrual irregularities
- Depression or low mood
- Slow heart rate
Hypothyroidism may result from several causes, including autoimmune thyroiditis (Hashimoto’s), iodine deficiency, or surgical removal of the thyroid. However, Hashimoto’s remains the leading cause in developed countries.
Hyperthyroidism (Overactive Thyroid)
Hyperthyroidism involves excessive thyroid hormone production. As a result, bodily systems speed up, and one may experience a range of symptoms that can disrupt daily life.
Common symptoms include:
- Weight loss despite a normal or increased appetite
- Heat intolerance and excessive sweating
- Rapid or irregular heartbeat
- Nervousness, anxiety, irritability
- Tremors in the hands or fingers
- Difficulty sleeping
- Diarrhea or frequent bowel movements
- Menstrual irregularities
In women, the most common cause of hyperthyroidism is Graves’ disease, an autoimmune condition in which antibodies stimulate the thyroid to produce excess hormones. Hyperthyroidism can lead to complications such as heart problems and bone density loss if left untreated.
Hashimoto’s Thyroiditis
Hashimoto’s Thyroiditis is an autoimmune disorder where the body’s immune system mistakenly attacks the thyroid gland. Over time, the thyroid becomes damaged and struggles to produce sufficient hormones, leading to hypothyroidism. Women with Hashimoto’s may initially present with mild hyperthyroidism symptoms before transitioning to an underactive state.
Key points about Hashimoto’s:
- Strong genetic predisposition and family history
- More prevalent in women than men
- Often coexists with other autoimmune disorders (e.g., celiac disease, type 1 diabetes)
- Tends to manifest with fluctuating thyroid hormone levels
Graves’ Disease
Graves’ disease is an autoimmune condition causing hyperthyroidism. It differs from Hashimoto’s in the type of antibody (Thyroid Stimulating Immunoglobulin, TSI) involved. This antibody overstimulates the thyroid gland, causing an overproduction of hormones.
Characteristic features of Graves’ disease include:
- Overactive thyroid (hyperthyroidism)
- Possible eye complications, known as Graves’ ophthalmopathy (eye bulging, irritation, dryness)
- Enlarged thyroid (goiter)
- Potential for weight loss, heart palpitations, insomnia
Postpartum Thyroiditis
Postpartum thyroiditis affects some women following childbirth. It typically unfolds in two phases:
- A hyperthyroid phase, where the thyroid releases excess stored hormones.
- A hypothyroid phase, as hormone levels drop.
Symptoms often mimic typical postpartum changes, making it hard to diagnose without testing. While many women recover normal thyroid function, some may progress to long-term hypothyroidism.
Thyroid Nodules and Goiter
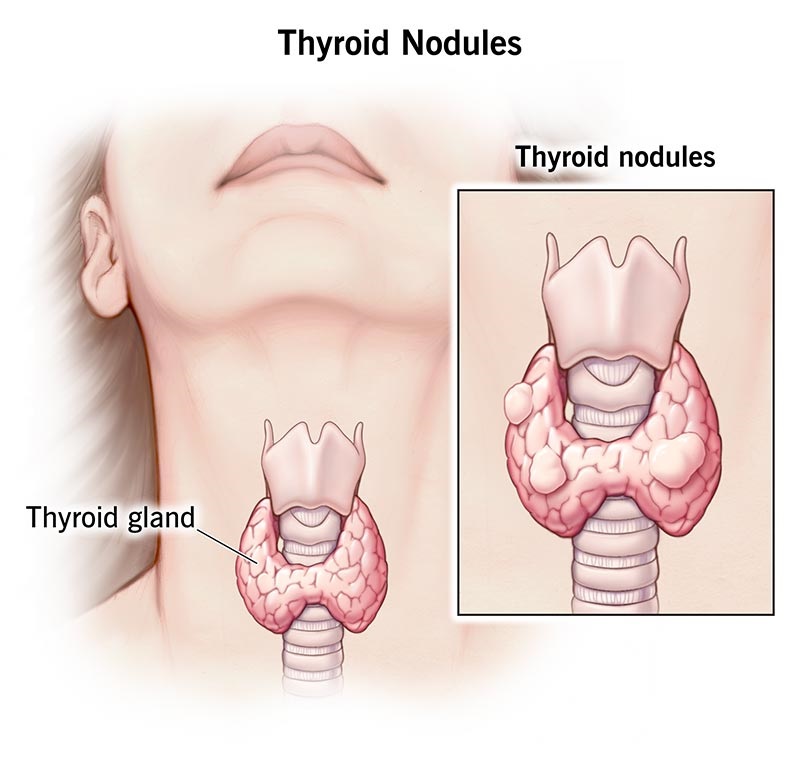
Thyroid nodules are lumps within the thyroid gland, which can be solid or fluid-filled. While most are benign, they can sometimes produce extra thyroid hormone, leading to hyperthyroidism, or they may develop into thyroid cancer in rare cases.
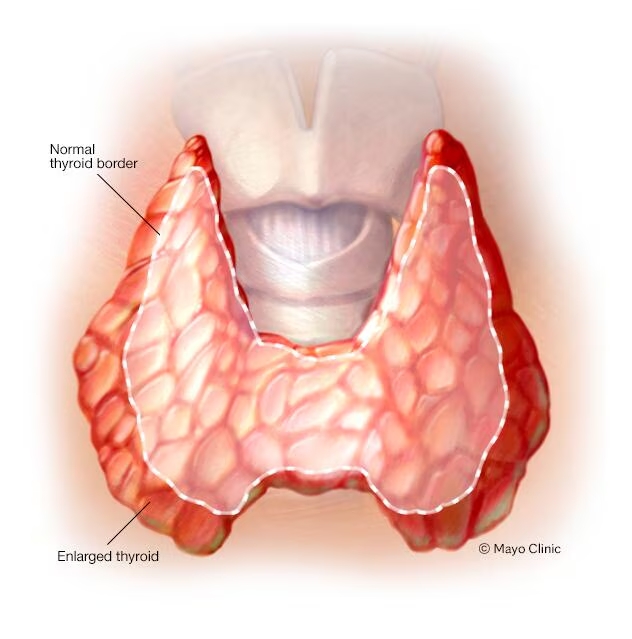
Goiter refers to an enlarged thyroid gland, which can occur in both hypothyroid and hyperthyroid conditions. Iodine deficiency is a frequent cause of goiter worldwide.
The Role of Iodine in Thyroid Function

Iodine Basics
Iodine is an essential trace mineral that the thyroid gland uses to produce T4 and T3. Without sufficient iodine, the thyroid cannot synthesize enough hormones, increasing the likelihood of hypothyroidism and goiter. Iodine deficiency remains a global issue, despite public health measures like iodized salt.
Key functions of iodine include:
- Building block for T3 and T4 hormone molecules
- Supports healthy thyroid tissue structure
- Helps maintain metabolism and energy levels
Daily Iodine Requirements for Women
For adult women, the Recommended Dietary Allowance (RDA) for iodine is approximately 150 micrograms (mcg) per day. This requirement increases during pregnancy and lactation to around 220-290 mcg per day because iodine is crucial for fetal brain development and for maintaining the mother’s own thyroid balance.
Iodine-Rich Foods

To maintain adequate iodine levels, focus on incorporating the following foods into your diet:
- Seafood: Fish, shellfish, and seaweed (e.g., kelp, nori) are excellent sources of iodine.
- Dairy products: Milk, cheese, and yogurt can be good iodine sources if animals receive iodine-fortified feed.
- Eggs: Egg yolks contain iodine if the hens are fed iodine-rich diets.
- Iodized salt: Table salt fortified with iodine (check the product label to verify).
Example: A sushi roll containing seaweed (nori) and fish can provide substantial iodine. However, you should also account for salt intake guidelines and not exceed recommended sodium levels.
Risks of Iodine Deficiency and Excess
Deficiency risks:
- Hypothyroidism
- Goiter formation
- Pregnancy complications (e.g., cretinism in infants)
- Increased risk of miscarriage or stillbirth
Excessive intake risks:
- Hyperthyroidism or hypothyroidism in susceptible individuals
- Possible thyroiditis
- Interference with medications
Maintaining iodine within recommended ranges is essential. Over-supplementing without professional guidance can trigger or exacerbate existing thyroid conditions, especially in the context of autoimmune thyroid disease.
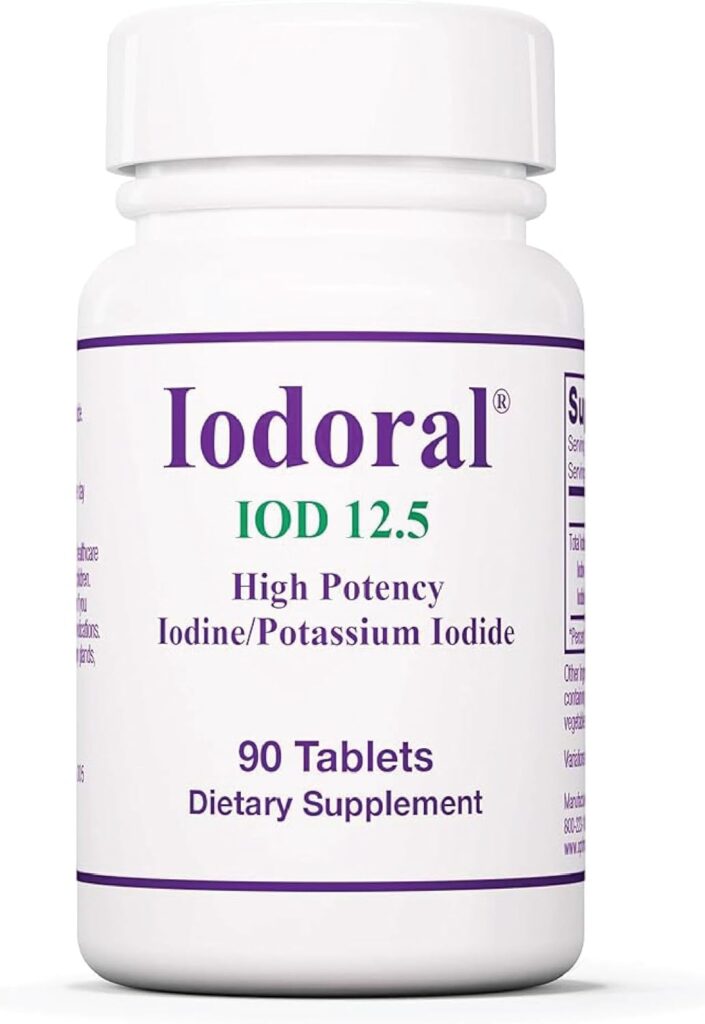
Iodine Supplementation Tips
- Consult a healthcare provider: Before adding an iodine supplement, discuss your health profile, existing thyroid status, and dietary intake with a medical professional.
- Follow dosage guidelines: Aim for around 150 mcg per day (for non-pregnant, non-lactating women) unless advised otherwise by your healthcare practitioner.
- Avoid mega-dosing: High doses of iodine (over 1,100 mcg per day for adults) can negatively impact thyroid function and overall health.
- Combine with selenium: Selenium helps in converting T4 to T3 and may reduce thyroid autoimmunity when used appropriately.
Herbal Support for Thyroid Health

Herbal medicine can complement conventional thyroid treatments, offering additional support for regulating hormones, reducing inflammation, and balancing the immune system. However, herbs should be used wisely and in consultation with a qualified practitioner—particularly if you’re on prescription thyroid medication.
Adaptogens for Thyroid Health
Adaptogens are herbs that help the body adapt to stress and maintain homeostasis. Chronic stress can dysregulate the hypothalamic-pituitary-adrenal (HPA) axis and, by extension, the thyroid axis. Incorporating adaptogens can potentially enhance resilience and modulate thyroid function.
- Ashwagandha (Withania somnifera): Known for its ability to support endocrine function, including thyroid balance. Preliminary research suggests it may help boost T4 levels in subclinical hypothyroid patients. However, caution is advised in cases of hyperthyroidism.
- Rhodiola rosea: Helps improve energy, mental focus, and reduce fatigue. Might support people experiencing stress-related thyroid imbalances.
Specific Herbs for Hypothyroidism

- Bladderwrack (Fucus vesiculosus): A seaweed known for its iodine content, bladderwrack is sometimes used to support low thyroid function. However, the iodine content can vary significantly, and excessive intake could lead to hyperthyroidism or thyroid irritation.

- Guggul (Commiphora mukul): A resin from the mukul tree that may support healthy T3 conversion. Some supplements combine guggul with other thyroid-supportive nutrients or herbs.
- Ashwagandha: As mentioned, can help normalize thyroid hormone levels and reduce stress.
Specific Herbs for Hyperthyroidism

- Lemon Balm (Melissa officinalis): Traditionally used to calm the nervous system and may help moderate thyroid hormone overproduction by impacting TSH receptor binding.

- Bugleweed (Lycopus virginicus): Often recommended for mild hyperthyroidism. It may help reduce excessive T4 production. Requires caution and guidance from a knowledgeable herbalist or healthcare provider because it can lower thyroid hormone levels significantly.

- Motherwort (Leonurus cardiaca): Known for its calming effect on heart palpitations, which is a common hyperthyroid symptom. It does not necessarily reduce thyroid hormone production but helps alleviate symptomatic discomfort.
Combining Herbal Support with Conventional Treatment
If you are on levothyroxine (T4 medication) or other prescription thyroid drugs, carefully monitor how herbs might interact with your regimen. For example, certain herbs high in iodine can interfere with T4 medication absorption or potency. Always inform your endocrinologist or primary care physician about any herbal supplements you are taking.
Practical tips:
- Start with low doses of any new herb and observe changes in energy, mood, and physical symptoms.
- Work with a practitioner to perform regular blood tests and confirm that your thyroid hormone levels remain in the optimal range.
- Check for potential side effects or allergies, especially if you have a history of autoimmune disorders.
Safety Considerations and Dosage
- Herb quality: Choose reputable brands that conduct quality testing to avoid contamination with heavy metals, pesticides, or adulterants.
- Individual variability: Responses to herbs differ from person to person due to genetics, lifestyle, and overall health.
- Autoimmune caution: Some herbs can stimulate or suppress immune function, so consult with a specialist if you have autoimmune thyroid disease.
Women’s Thyroid Symptom Checker

A thyroid imbalance can sometimes be elusive. Many symptoms overlap with other conditions, and the presentation can vary significantly among women. Below is a comprehensive symptom checker to help you recognize potential thyroid issues. Use this as a guide to prompt further evaluation but remember it is not a substitute for professional diagnosis.
Early Warning Signs
- Unexplained weight changes: Sudden gain or loss despite unchanged diet or exercise habits.
- Fatigue or insomnia: Persistent daytime drowsiness or insomnia at night, especially if it’s a new development.
- Mood swings: Anxiety, irritability, or depression that doesn’t seem tied to external factors.
- Brittle hair and nails: Thinning or breaking hair, peeling nails.
- Dry skin or excessive sweating: Skin changes are often an early sign of hormone imbalance.
Hypothyroid Symptom List
- Slow metabolism, leading to easy weight gain
- Sensitivity to cold temperatures
- Slow, sluggish feeling, fatigue
- Constipation or difficulty with bowel movements
- Slow heart rate, potential for elevated cholesterol
- Menstrual irregularities (heavy or prolonged bleeding)
- Brain fog, memory issues
- Joint or muscle pain without obvious cause
Hyperthyroid Symptom List
- Rapid weight loss or inability to gain weight
- Heat intolerance, feeling excessively warm
- Racing heart, palpitations, or arrhythmias
- Irritability, nervous energy, anxiety
- Frequent bowel movements or diarrhea
- Sweaty, clammy skin
- Light or irregular menstrual periods
- Hand tremors, muscle weakness
Menstrual and Fertility-Related Symptoms
Thyroid hormones significantly impact reproductive health. Women with thyroid imbalances may experience:
- Irregular cycles: Lengthening or shortening of the cycle, unpredictable bleeding.
- Heavy or scanty periods: Hypothyroidism can cause heavier flows, while hyperthyroidism may lighten periods.
- Infertility or difficulty conceiving: Both hypo- and hyperthyroidism can disrupt ovulation.
- Pregnancy complications: Untreated thyroid disorders can lead to miscarriage, preterm labor, or low birth weight.
Lifestyle and Mental Health Indicators
- Energy crashes: Needing frequent naps or feeling lethargic throughout the day.
- Exercise intolerance: Difficulty recovering from workouts, shortness of breath, or heart palpitations.
- Hair thinning or loss in patches: Can be a sign of both hypo- and hyperthyroidism.
- Anxiety or depression: Thyroid hormone fluctuations can trigger or worsen mood disorders.
- Reduced libido: Decreased sex drive can result from disrupted hormones.
When to Seek Professional Advice
- If you have multiple persistent symptoms from the lists above.
- Notable changes in menstrual cycle regularity.
- Sudden weight fluctuations without changes in diet or exercise.
- Heart palpitations, tremors, or shortness of breath.
- Unexplained fatigue, depression, or mood swings.
If any of these symptoms persist for several weeks or worsen, schedule a medical appointment for a comprehensive thyroid evaluation.
Additional Nutritional and Lifestyle Considerations

Essential Nutrients Beyond Iodine
While iodine is paramount for thyroid hormone synthesis, other nutrients also play significant roles in thyroid health:
- Selenium: Needed for converting T4 to T3 and for supporting thyroid antioxidant defenses. Sources include Brazil nuts, sunflower seeds, and seafood.
- Zinc: Involved in thyroid hormone metabolism. Found in oysters, pumpkin seeds, and beef.
- Iron: Low iron levels can impair thyroid hormone synthesis. Ensure adequate intake through lean meats, beans, and leafy greens.
- Vitamin D: Autoimmune thyroid conditions often coexist with vitamin D deficiency. Sunlight exposure and supplementation can help maintain optimal levels.
- B Vitamins: Critical for energy metabolism and cellular function. Foods like whole grains, meat, eggs, and legumes are rich in these vitamins.
The Impact of Stress on Thyroid Health
Chronic stress elevates cortisol levels, which can disrupt the HPA axis and reduce the conversion of T4 to T3. High cortisol may also contribute to autoimmune flare-ups. Incorporating stress management techniques—such as meditation, yoga, or journaling—can significantly support thyroid function.
Example stress-relief practices:
- Deep breathing exercises: Slow, diaphragmatic breathing to activate the parasympathetic nervous system.
- Regular breaks: Incorporate short walks or stretching routines during the workday.
- Mindfulness and meditation apps: Use guided meditations to calm the mind.
Dietary Tips for Thyroid Care
- Balance macronutrients: Focus on proteins (lean meats, beans), healthy fats (avocados, nuts, seeds), and complex carbohydrates (whole grains, vegetables).
- Avoid excessive goitrogens: Foods like cruciferous vegetables (kale, broccoli) contain goitrogens. While they are nutritious and generally safe in moderation, excessive amounts may interfere with iodine uptake in individuals with iodine deficiency or existing thyroid issues. Cooking these vegetables typically reduces their goitrogenic properties.
- Limit processed foods: Refined sugars and unhealthy fats can fuel inflammation and disrupt hormonal balance.
- Moderate caffeine and alcohol intake: Both can exacerbate anxiety, sleep disturbances, or interfere with thyroid medication.
Exercise and Weight Management
Physical activity supports metabolism, mood balance, and cardiovascular health—key areas impacted by thyroid function. Aim for a consistent exercise routine tailored to your energy levels:
- Low-impact exercises: Yoga, Pilates, or brisk walking for hypothyroid patients who struggle with fatigue or joint pain.
- Moderate to high-intensity workouts: For hyperthyroid individuals, ensure you are cleared by a doctor, especially if you experience heart palpitations.
- Gradual progression: Increase intensity slowly, monitoring how your body responds.
Testing, Diagnosis, and Working with Your Healthcare Provider

Thyroid Function Tests
Blood tests remain the gold standard for diagnosing thyroid disorders. Key tests include:
- TSH (Thyroid Stimulating Hormone): The primary screening test. High TSH usually indicates hypothyroidism, while low TSH may signify hyperthyroidism.
- Free T4 (Free Thyroxine): Shows the level of unbound T4 hormone available in the blood.
- Free T3 (Free Triiodothyronine): Reflects the amount of active thyroid hormone. Low T3 can occur even if T4 is normal.
- Reverse T3 (rT3): Helps identify conversion issues from T4 to T3.
Interpreting Lab Results
Optimal thyroid function goes beyond being within the “normal range.” Many practitioners use more functional or optimal ranges, slightly narrower than standard lab references, to detect subclinical thyroid issues that can still cause symptoms.
Example of typical reference ranges:
- TSH: Approximately 0.5–5.0 mIU/L (depending on the lab)
- Free T4: ~0.9–1.7 ng/dL
- Free T3: ~2.0–4.4 pg/mL
Because these ranges vary by laboratory, always discuss your results with a knowledgeable provider who can integrate lab data with your symptoms.
Antibody Testing
For autoimmune thyroid disorders, antibody testing is crucial:
- Thyroid Peroxidase Antibodies (TPOAb): Commonly elevated in Hashimoto’s thyroiditis.
- Thyroglobulin Antibodies (TgAb): Another marker for autoimmune activity.
- Thyroid Stimulating Immunoglobulin (TSI): Elevated in Graves’ disease.
Imaging and Ultrasound
If you have a goiter or nodules, an ultrasound can help assess thyroid gland structure, nodule characteristics, and blood flow. Nodules suspected of malignancy may require a fine-needle aspiration biopsy.
Collaborating with a Thyroid-Savvy Practitioner
Finding a healthcare provider well-versed in thyroid disorders is essential for proper diagnosis and management. You may consider an endocrinologist, an integrative or functional medicine practitioner, or a naturopathic doctor specializing in endocrine health.
Tips for productive healthcare visits:
- Keep a journal of symptoms, diet, and lifestyle factors.
- Bring any relevant lab reports or imaging results.
- Ask specific questions about medication options, supplementation, and monitoring frequency.
Practical Tips for Ongoing Thyroid Care
How to Track Symptoms
Maintaining a health journal can be a powerful tool in identifying thyroid fluctuations:
- Record daily energy levels, mood, and sleep patterns.
- Note any new or worsening symptoms (hair loss, weight changes, palpitations).
- Keep track of your menstrual cycle specifics (length, heaviness, pain).
Maintaining a Balanced Lifestyle
- Sleep hygiene: Aim for 7-9 hours of quality sleep. Inadequate rest can skew hormone levels and amplify stress.
- Stress management: Incorporate mindfulness practices, physical relaxation techniques, and social support.
- Routine medical checkups: Even if you feel well, schedule periodic thyroid function tests to detect subtle changes.
Long-Term Management Strategies
- Medication adherence: If prescribed thyroid hormone replacement, take it consistently at the same time each day, preferably on an empty stomach.
- Regular labs: Test TSH, Free T4, Free T3, and antibodies as recommended by your provider.
- Dietary adjustments: Revisit iodine intake, ensure balanced nutrients, and limit inflammatory foods.
- Herbal rotations: If you use herbal supplements, evaluate their effectiveness and safety over time, rotating or adjusting as needed under professional guidance.
Conclusion
A healthy thyroid is fundamental to women’s well-being, affecting metabolism, energy, mood, and reproductive health. By understanding the complex interactions of thyroid hormones, recognizing early symptoms, and seeking timely professional care, you can better ensure optimal thyroid function through all stages of life.
Key takeaways from this comprehensive guide:
- The thyroid drives metabolic and hormonal balance. Women, in particular, are susceptible to thyroid imbalances due to shifts in reproductive hormones and a higher propensity for autoimmune disorders.
- Iodine is critical but should be handled cautiously. Both deficiency and excess can lead to thyroid dysfunction. Dietary sources or targeted supplementation must be carefully managed.
- Herbal and natural remedies offer supportive care. Adaptogens like ashwagandha can alleviate stress, while herbs like lemon balm and bugleweed may help modulate thyroid activity. However, always consult professionals about potential interactions with medications.
- Symptom awareness is vital. Keep an eye out for signs of both hypo- and hyperthyroidism. Use a symptom checker and track menstrual irregularities, energy levels, and weight changes.
- Lifestyle factors matter. Nutrition, stress management, and regular exercise can significantly influence thyroid health.
- Regular testing and professional collaboration are paramount. Ensure TSH, Free T4, and Free T3 are regularly monitored, especially during pregnancy or if you have a known autoimmune condition.
Ultimately, a combination of evidence-based medical care, informed nutritional choices, mindful lifestyle practices, and strategic herbal support can help you maintain robust thyroid health. If you suspect a thyroid issue or are experiencing persistent symptoms, reach out to a qualified healthcare provider for testing and personalized guidance. Your thyroid is not just a small gland in your neck—it’s a critical conductor of your body’s symphony, deserving of informed, proactive care.