Ever roll out of bed already wiped, hunt down sugary snacks by lunchtime, and then stare at the ceiling with your thoughts on turbo-drive at night? That daily roller-coaster usually points to hormones running the show: cortisol cranked up, thyroid idling, or estrogen and progesterone dancing out of sync.
Sure, meds can help—but they’re not the only game in town. A growing stack of research (and centuries of tradition) says certain herbs can gently steer things back toward natural hormone balance, easing weight creep and mood swings without the usual pill-box side effects.
Below, you’ll get a quick-read playbook: what the studies say, how much to take, and easy lifestyle tweaks. Skim it once, keep it handy, and start feeling steady energy, a lighter mind, and a metabolism that’s actually on your side.
Why Balanced Hormones Matters for Body Fat & Brain Chemistry
Hormones are your body’s push-notifications: tiny biochemical messages that tell every cell when to burn calories, store them, or spin up mood-lifting neurotransmitters. Miss a few of those pings—or get spammed—and both your waistline and mindset start to drift.
Below is a closer look at the headline players, the latest science on how they tilt weight and mood, and the hidden ways they interact with one another.
Cortisol — “The Stress Guardian”
When you’re late for a deadline, a cortisol surge mobilises glucose and sharpens focus—helpful in short bursts. Trouble begins when the alert never shuts off. Chronic elevation triggers visceral-fat deposition (the deep “danger fat” around organs) and physically shrinks hippocampal sub-regions linked to memory and mood regulation.MRI studies show that higher long-term cortisol (measured in hair samples) correlates with smaller CA1–3 and dentate-gyrus volumes; lowering cortisol through lifestyle change can reverse some of that loss. (PMC, PubMed)
Metabolically, persistent cortisol also makes fat cells hoard calories, worsens insulin resistance, and raises inflammatory cytokines—an internal setting that practically “pre-orders” abdominal weight gain while priming the brain for anxiety and depression. (PMC)
Insulin — “The Energy Broker”
Every time you eat carbohydrate, insulin escorts glucose into muscle and liver for immediate use or storage. Chronically high intake of refined carbs, seed-oil–rich ultra-processed foods, or simply frequent snacking means insulin is elevated so often that cells stop answering the door—a state called insulin resistance. Blood sugar stays high, gets converted to fat, and—importantly—starves the brain of glucose. Emerging research shows that people with obesity or type-2 diabetes can have lower brain-glucose levels than lean individuals, resulting in fatigue and the “brain fog” many low-carb dieters notice during adaptation. (Frontiers)
Left unchecked, insulin resistance feeds back into cortisol overproduction (your body sees fluctuating sugar as stress) and encourages more fat storage, creating a vicious loop.
Thyroid Hormones (T3 & T4) — “The Metabolic Thermostat”

Thyroxine (T4) and its active form triiodothyronine (T3) set your basal metabolic rate—the calories you burn just by existing. Even a 5 % drop in free T3 can add several kilos per year without any change in diet. Subclinical hypothyroidism is increasingly tied to obesity, and multiple population studies confirm a bidirectional link between low thyroid function and depression or anxiety; women are particularly vulnerable. (PMC, Wiley Online Library)
Because cortisol blunts conversion of T4 → T3, chronic stress can masquerade as thyroid sluggishness. That’s why supporting adrenal balance (sleep, adaptogens) often improves thyroid labs and lifts mood.
Sex Hormones — Estrogen, Progesterone & Testosterone
Balanced ratios of these hormones stabilise dopamine and serotonin, maintain lean muscle, and keep cravings in check. Disruption can run two ways:
- Estrogen dominance (excess estrogen relative to progesterone) promotes water retention, dysregulated hunger signals, and belly-fat storage; adipose tissue then produces more estrogen, locking in the cycle. (MDPI, Plate and Canvas)
- Low testosterone in men (and women) reduces muscle mass, slows resting metabolism, and is associated with irritability and low drive.
Mood swings are common on both sides of the imbalance because estrogen and testosterone modulate key neurotransmitter pathways.
Appetite & Gut-Brain Hormones — GLP-1, Leptin, Ghrelin, Serotonin, GABA
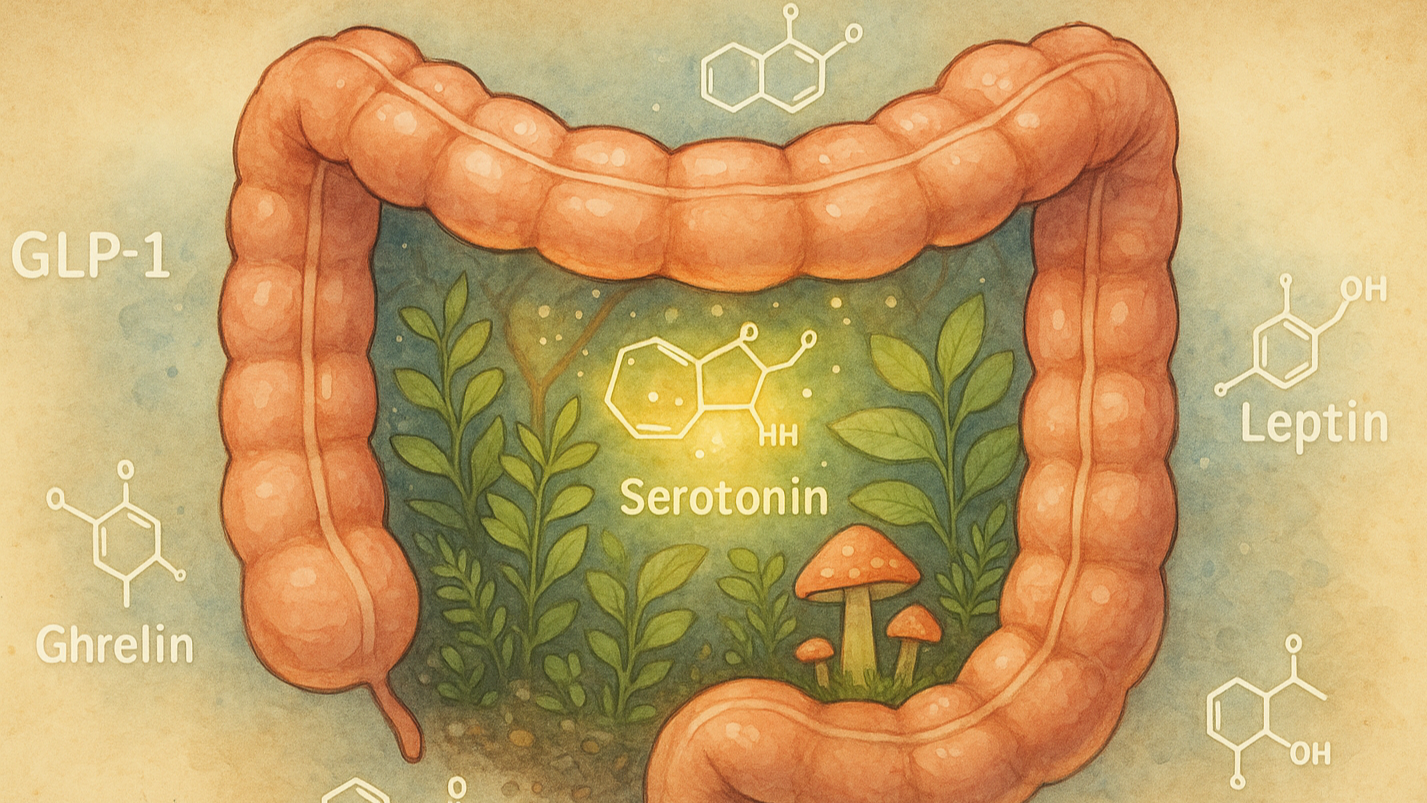
Your digestive tract is not just a food-processing tube; it’s an endocrine powerhouse.
- Serotonin: About 90 % is synthesised in gut enterochromaffin cells under the influence of resident microbes. Dysbiosis disrupts this supply line, which can translate into both depressive symptoms and erratic bowel habits. (PMC, Nature)
- GLP-1 & PYY: These peptides slow gastric emptying and tell the brain you’re full. Current GLP-1 agonist drugs prove how powerful the pathway is, but lifestyle factors such as fibre-rich diets and strength training also boost endogenous GLP-1. (Nutritional Outlook)
- Leptin & Ghrelin: Think of leptin as “I’m satisfied” and ghrelin as “Feed me now.” Short sleep or high stress drops leptin and spikes ghrelin, pushing midnight snacking and weight gain. (Nature, Health)
Because these gut-derived signals cross-talk with cortisol, insulin, and sex hormones, a disrupted microbiome or chronically irregular sleep schedule sends ripples through every other system.
Why One Hormone Rarely Misbehaves Alone
Imagine the endocrine network as a jazz ensemble: when the drummer (cortisol) speeds up, the bass (insulin) compensates, the horns (thyroid) fall out of rhythm, and the vocalist (neurotransmitters) can’t hold the tune. That’s why spot-treating only one hormone—say, taking thyroid meds without addressing stress or diet—often yields partial results. Holistic approaches that calm the HPA axis, improve insulin sensitivity, nurture gut bacteria, and restore sleep can bring the entire band back in sync faster than isolated fixes.
Key takeaway: Your hunger, fat distribution, and emotional resilience are co-authored by this hormonal cast. Balancing them demands a systems mindset—leveraging food quality, circadian-aligned habits, and targeted botanicals—to create harmony rather than silencing a single instrument.
Why Herbs for Balanced Hormones?

Plants are master chemists. Over millions of years they have evolved thousands of secondary metabolites—adaptogenic saponins, phytoestrogens, terpenes, flavonoids, alkaloids—that slip into human receptor sites the way a key fits a lock. Whereas a synthetic drug often hammers a single pathway, botanicals practice “network pharmacology.” They nudge multiple signaling cascades—HPA-axis tone, insulin sensitivity, gut–brain peptides—so your own endocrine system can finish the job of self-regulation.
Recent meta-analyses confirm that classic adaptogens (ashwagandha, rhodiola, eleuthero) raise stress resilience without the sedation or tolerance seen with many anxiolytics.
Why reach for herbs first?
- Gentler safety margin. Most hormone-active botanicals have centuries of culinary or ritual use; modern trials back that up. Black cohosh, for instance, shows no serious adverse events across 12-month studies, while lemon balm’s LD₅₀ is orders of magnitude above typical doses.
- Built-in synergy with healthy habits. Ashwagandha’s cortisol-lowering effect enhances the glucose control you get from strength training; bitter herbs like dandelion amplify the fiber-driven boost to GLP-1 after a veggie-rich meal. Herbs make good habits work harder.
- Microbiome cross-talk. Polyphenols from holy basil or artichoke leaf feed Bifidobacteria and Akkermansia, which in turn generate short-chain fatty acids that steady insulin and leptin signaling. Few pharmaceuticals offer that two-way gut–hormone benefit.
- Accessibility and cost. Standardized capsules, tinctures, or bulk teas are inexpensive, shelf-stable, and often legal to grow at home—holy basil or lemon balm thrive in a balcony pot.
- Personalization. Because herbs modulate rather than override, they can be stacked or rotated—vitex for luteal-phase mood swings, rhodiola for high-intensity training blocks, lemon balm for evenings—allowing you to fine-tune regimens as labs and symptoms evolve.
- Sustainability. Cultivating perennials like ashwagandha and maca can be less resource-intensive—and more biodiversity-friendly—than synthesizing petrochemical-derived pharmaceuticals.
Key takeaway: Herbs are arguably nature’s built-in endocrine toolkit—versatile, synergistic, and friendly to long-term use—making them a smart first line (or companion) for anyone seeking hormone harmony without heavy pharmacologic baggage.
Herbs for Balanced Hormones
Below you’ll find the heavy-hitters, each backed by peer-reviewed studies or authoritative monographs. Suggested dosage ranges reflect typical research protocols; start low and titrate slowly.
1. Ashwagandha (Withania somnifera): Stress-Blocker & Thyroid Ally

- Primary actions: Adaptogen; lowers cortisol; may boost conversion of T4 → T3.
- Key findings: A 2024 NIH factsheet summarizes multiple trials where daily ashwagandha (300–600 mg root extract) cut cortisol by up to 30 percent and significantly reduced anxiety scores. (Office of Dietary Supplements) Another meta-analysis noted improved VO₂ max and lower serum cortisol, linking it indirectly to better weight management and mood. (PMC)
- Dosing guide: 300 mg standardized to ≥5 percent withanolides, twice daily with food.
- Who benefits most: Stressed overeaters, night-owl entrepreneurs, women with “adrenal belly,” people coming off high-intensity training blocks.
2. Holy Basil (Ocimum sanctum, Tulsi): Cortisol Calmer & Blood-Sugar Buffer

- Primary actions: Modulates HPA axis; improves insulin sensitivity; anti-inflammatory.
- Key findings: Recent reviews (2023–2024) credit eugenol and ursolic acid with normalizing morning cortisol and lowering fasting glucose, indirectly aiding fat loss and emotional stability. (Dr. Jolene Brighten, News-Medical)
- Dosing guide: 400–600 mg leaf extract (2% ursolic acid) once or twice daily; or 2–3 cups of Tulsi tea.
- Pro tip: Pair with ½ tsp Ceylon cinnamon to further blunt post-meal glucose spikes.
3. Vitex Agnus-Castus (Chasteberry): Progesterone Promoter & PMS Peacemaker

- Primary actions: Lowers elevated prolactin; shifts estrogen-progesterone ratio, easing water retention and irritability.
- Key findings: Clinical data support symptom relief in PMS, PMDD, and perimenopause; anecdotal evidence shows improved cycle regularity in PCOS, aiding weight management. (Healthline)
- Dosing guide: 20–40 mg standardized fruit extract, AM only (pituitary is most responsive then).
- Watch-outs: Avoid during hormonal contraceptives unless supervised; may affect fertility.
4. Black Cohosh (Cimicifuga racemosa): Menopause Weight-Gain Shield

- Primary actions: Acts on serotonin and possibly estrogen receptors to reduce vasomotor symptoms, improve sleep, and curb emotional eating.
- Key findings: Three of four randomized trials in a 2024 meta-analysis found black cohosh superior to placebo for menopausal symptom scores. (Lippincott Journals) Sleep improvements alone can reverse leptin-ghrelin imbalances that drive late-night snacking.
- Dosing guide: 40 mg root/rhizome extract (2.5% triterpene glycosides) daily.
- Safety: Research up to one year shows good tolerance; rare cases of liver upset—monitor if you have hepatic issues. (NCCIH)
5. Lemon Balm (Melissa officinalis): GABA Booster for Anxious Cravings

- Primary actions: Inhibits GABA-transaminase, raising calming neurotransmitter levels; mild thyroid-modulating effect.
- Key findings: A placebo-controlled trial in 200 adolescents saw 1,200 mg/day slash anxiety, depression, and insomnia scores over three cycles—demonstrating both psychological and hormonal benefit. (PMC)
- Dosing guide: 300 mg extract up to four times daily or 2 g dried herb infused as tea.
- Mood hack: Combine with magnesium glycinate in the evening for deeper REM sleep and improved morning insulin sensitivity.
6. Bonus Adaptogens: Rhodiola & Maca


Even though robust hormone-specific trials are fewer, these staples deserve mention. Rhodiola rosea improves perceived exertion and may blunt cortisol rise during high-intensity workouts, while Lepidium meyenii (maca) shows promise in balancing libido-related hormones and lifting mood. Both reinforce the adrenal-thyroid-gonadal axis synergy touted by adaptogen research. (News-Medical)
7. Gut-Brain Herbs: Prebiotic Bitters & Polyphenol Power



A healthy microbiome manufactures weight-regulating peptides (GLP-1, PYY) and roughly 90 percent of the body’s serotonin. Herbs such as artichoke leaf, dandelion root, and bitter melon feed beneficial bacteria, boosting metabolic health and mental resilience. Emerging microbiota-targeted therapies—including herbal synbiotics—reduce obesity indicators and insulin resistance. (PMC)
Hormone-Friendly Daily Routine
1. Sunrise Light (within 30 min of waking)

Step outside—or at least sit by an open window—without sunglasses for 5-10 minutes. The strong blue-wavelength light spikes cortisol early (where it belongs), locks your circadian clock, and nudges daytime serotonin so you feel alert without extra caffeine.
2. Protein-Powered Breakfast (30-60 min after light)
Aim for 30 g of protein: think three eggs with avocado, a scoop of whey in your coffee, or a tofu-seed scramble. Solid protein triggers GLP-1 and PYY to keep you full, blunts the insulin surge that causes mid-morning crashes, and supplies amino acids for thyroid and dopamine production.
3. First Herb Window (take with breakfast)

• Ashwagandha 300 mg lowers excess cortisol.
• Vitex 20 mg (or 40 mg black cohosh if perimenopausal) balances progesterone and prolactin.
Swallow capsules with a little dietary fat to boost absorption.
4. Ten-Minute Movement Snack (right after breakfast)

Walk around the block, bang out 20 body-weight squats, or do a set of desk push-ups. That quick muscle work opens GLUT-4 channels so glucose slides into muscle without calling for extra insulin—up to a 30 % cut in the meal’s blood-sugar hit.
5. Mid-Afternoon Stress Reset (~3 p.m.)

Brew a cup of holy basil (tulsi) tea—about 400 mg leaf extract. While it steeps, take five slow diaphragmatic breaths (4-second inhale, 6-second exhale). Tulsi calms the HPA axis, and deep breathing spikes heart-rate variability, flattening the cortisol bump that drives 3 p.m. sugar cravings.
6. Strength or HIIT Session (late afternoon, 4-7 p.m.)

Lift weights for 30 minutes or hit a 15-minute kettlebell/HIIT circuit. Resistance work makes muscles voracious for glucose for the next 24 hours, spikes growth hormone and testosterone, and paradoxically deepens your night-time sleep.
7. Balanced Dinner (finish ≥2 h before bed)

Plate up lean protein, fiber-heavy veggies, and a resistant-starch carb like cooled rice or lentils. This combo steadies nighttime blood sugar, feeds gut microbes that produce serotonin, and supports healthy leptin signaling so late-night munchies stay quiet.
8. Evening Wind-Down (1 h before bed)

Sip 300 mg lemon-balm tea, switch on an amber screen filter, and roll through 10 minutes of gentle yoga or legs-up-the-wall. Optional bonus: 400 mg magnesium glycinate. Lemon balm raises calming GABA; magnesium soothes NMDA receptors, together dialing cortisol down for sleep.
9. Consistent Sleep Window (7–9 h, same lights-out nightly)

Keep the room cool (<20 °C / 68 °F) and blackout-dark. Consistent bedtimes pin ghrelin (hunger) low, leptin high, and morning cortisol right on time—making restorative sleep the cheapest hormone therapy you’ll ever find.
Track energy, mood, and waist once a week. Tiny tweaks—catching morning light even on cloudy days, swapping herbs if cycles shift—compound into major hormonal harmony within a month or two.
Quality, Dosage & Safety

- Go for standardized extracts. The label should specify both plant part and active-compound percentage—e.g., “Ashwagandha root, 600 mg, ≥ 5 % withanolides (KSM-66).” Without those numbers potency can vary 10-fold between brands.
- Insist on third-party verification. Look for NSF Certified, USP Verified, or ConsumerLab approval on the bottle or the company’s website. These seals confirm the product is free of heavy metals, pesticides, and unlabeled fillers—common issues in cheaper imports.
- Respect dosing ranges. Adaptogens follow a hormetic curve: low-to-moderate doses trigger beneficial stress-response pathways; mega-dosing can blunt the effect or create new side-effects (e.g., ashwagandha GI upset above 1,000 mg/day).
- Check for drug interactions.
Chasteberry can raise dopamine and may alter the effect of antipsychotics.
Black cohosh has mild estrogenic action—use caution alongside HRT or tamoxifen.
Lemon balm potentiates sedatives and can lower thyroid hormones in high doses. When in doubt, run your supplement list past a pharmacist. - Cycle adaptogens for receptor “reset.” A practical rhythm: 8–12 weeks on, followed by a 2-week break. Track sleep, mood, and resting heart rate during the off phase; if benefits hold, you can restart or switch to a different adaptogen family.
- Storage & shelf life. Keep capsules in a cool, dark place and discard anything > 2 years old or that smells musty—oxidized herbs lose potency and may harbor mold.
FAQs
1. Can I use these herbs while on hormonal birth-control?
Most adaptogens are neutral, but chasteberry can lower contraceptive effectiveness by altering prolactin and LH levels. If you rely on the pill or IUD for contraception, skip chasteberry or get medical clearance first.
2. Are these herbs safe during pregnancy or breastfeeding?
Generally no. Ashwagandha, vitex, black cohosh, and rhodiola are contraindicated because they can influence uterine tone or hormone levels. Lemon balm and holy basil have limited safety data—err on the side of avoidance unless a qualified professional okays a small dose.
3. Do I have to cycle all herbs, or only adaptogens?
Cycle adaptogens (ashwagandha, rhodiola, holy basil, maca) every 8–12 weeks. Single-target herbs like lemon balm for sleep can be used continuously, but take a week off every quarter to check that benefits persist.
4. Can I combine these herbs with GLP-1 drugs such as semaglutide?
Usually yes, but start low. Holy basil and cinnamon can further lower blood glucose, so monitor for light-headedness and adjust carb intake or medication dose with your doctor’s guidance.
5. Which lab markers help me track progress?
Morning serum cortisol, HbA1c, fasting insulin, free T3/T4, and sex-hormone panels (estradiol, progesterone, testosterone). Pair labs with subjective logs—energy, mood, waist circumference—for a full picture.
6. Capsules vs. tinctures—does the form matter?
Standardized capsules deliver a precise dose and hide plant taste; alcohol tinctures absorb faster but vary batch to batch. For thyroid or cortisol work, stick to standardized capsules; for sleep herbs like lemon balm, tinctures are fine.
7. Do any of these herbs interfere with surgery or lab tests?
Rhodiola and holy basil can thin blood slightly; stop a week before surgery. Vitex may skew prolactin or progesterone readings—tell your clinician if you’ve used it in the past month.
8. Can teenagers use adaptogens safely?
Data are limited. Occasional lemon-balm tea for anxiety is generally safe, but potent endocrine modulators (ashwagandha, vitex, maca) should wait until after full pubertal development unless supervised by a pediatric specialist.
9. Will adaptogens give me caffeine-like jitters?
No—true adaptogens balance cortisol rather than spike adrenaline. If you feel wired, your dose is probably too high or you’re combining them with excess coffee; scale back and re-assess.
Conclusion
Hormone chaos doesn’t happen overnight, and neither does harmony. Yet within weeks, strategic botanical allies—combined with smart nutrition, movement, and restorative sleep—can lower stress, trim visceral fat, and clear mental fog. Start small: brew a tulsi-cinnamon tea tomorrow morning or swap doom-scrolling for lemon-balm-aided journaling tonight. The science is compelling, the tools are accessible, and the body is primed to heal when given the right signals. A more balanced, energetic, and emotionally resilient you is only a dose (and a deep breath) away.