PCOS (Polycystic Ovary Syndrome) and PCOD (Polycystic Ovarian Disease) are two common hormonal conditions that affect the ovaries but they’re not exactly the same. While both involve issues like irregular periods, hormonal imbalances, and the presence of ovarian cysts, they differ in severity, long-term health risks, and how they impact the body over time.
The terms are often used interchangeably, especially in everyday conversations and even some medical circles. But knowing the difference is important especially for anyone experiencing symptoms, planning to conceive, or simply trying to understand their reproductive health better.
In this easy-to-follow guide, we’ll break down everything you need to know:
- What PCOS and PCOD actually are
- How they’re diagnosed
- The key differences between PCOS vs PCOD
- Symptoms to watch for
- Causes and risk factors
- Effective treatment and lifestyle changes
Whether you’ve been recently diagnosed or are just trying to make sense of these terms, this article will help you clearly understand the science behind PCOS and PCOD and what you can do to manage them better.
Table of Contents
How PCOS and PCOD Impact the Body
Both PCOS and PCOD are rooted in hormonal imbalances that can disrupt multiple systems in the body not just reproductive function. These conditions affect how the ovaries work, often leading to irregular menstrual cycles, ovulation issues, and a cascade of metabolic effects that go beyond fertility.
While symptoms and severity can vary, what makes these disorders particularly challenging is their connection to hormonal, metabolic, and inflammatory pathways. This means they can influence not only reproductive health, but also weight regulation, skin health, insulin function, and long-term risks like type 2 diabetes or cardiovascular disease.
Because these conditions develop gradually and can be overlooked for years, understanding their broader effects helps individuals recognize the signs earlier and seek timely support. In the sections that follow, we’ll explore the specific features of PCOS and PCOD, how they are diagnosed, and what makes them different from each other medically and practically.
What Is PCOS and How Does It Affect the Body?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects how the ovaries function. It’s one of the most common endocrine conditions in people of reproductive age and is often linked to irregular menstrual cycles, excess male hormones (androgens), and small fluid-filled sacs (or follicles) in the ovaries.
Despite the name, not everyone with PCOS actually has ovarian cysts and having cysts alone isn’t enough to diagnose the condition. PCOS is more about how your hormones behave than what your ovaries look like on an ultrasound.
Core Features of PCOS
- Hormonal Imbalance (Hyperandrogenism): Elevated androgens like testosterone can cause symptoms such as acne, unwanted facial or body hair (hirsutism), and thinning hair on the scalp.
- Irregular or Missed Periods: Many individuals with PCOS experience infrequent periods or no periods at all, due to problems with ovulation (anovulation).
- Ovarian Changes: The ovaries may appear enlarged and contain multiple small follicles that don’t mature into eggs, contributing to irregular cycles.
How PCOS Disrupts Hormonal Balance
PCOS is often associated with imbalances in key reproductive and metabolic hormones:
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) may be out of sync, disrupting ovulation.
- Insulin resistance is common, where the body doesn’t respond properly to insulin. This triggers higher insulin production, which in turn can raise androgen levels and worsen symptoms.
- This hormonal chaos can create a cycle of irregular menstruation, metabolic issues, and fertility challenges.
Potential Health Consequences
If left unmanaged, PCOS can increase the risk of:
- Type 2 diabetes
- High cholesterol and cardiovascular disease
- Endometrial hyperplasia (thickening of the uterine lining)
- Infertility due to chronic ovulation issues
When and How It’s Diagnosed
PCOS usually shows up during the late teens to early 30s, but it may go unnoticed until someone seeks help for irregular periods or difficulty getting pregnant.
Doctors often use the Rotterdam criteria for diagnosis, which requires at least two of the following:
- Irregular or absent ovulation
- Signs of high androgen levels (acne, hair growth, or elevated blood tests)
- Polycystic ovaries visible on an ultrasound
PCOS can’t be diagnosed through a single test it’s a diagnosis based on patterns in symptoms, hormone levels, and imaging.
What Is PCOD and How Is It Different From PCOS?
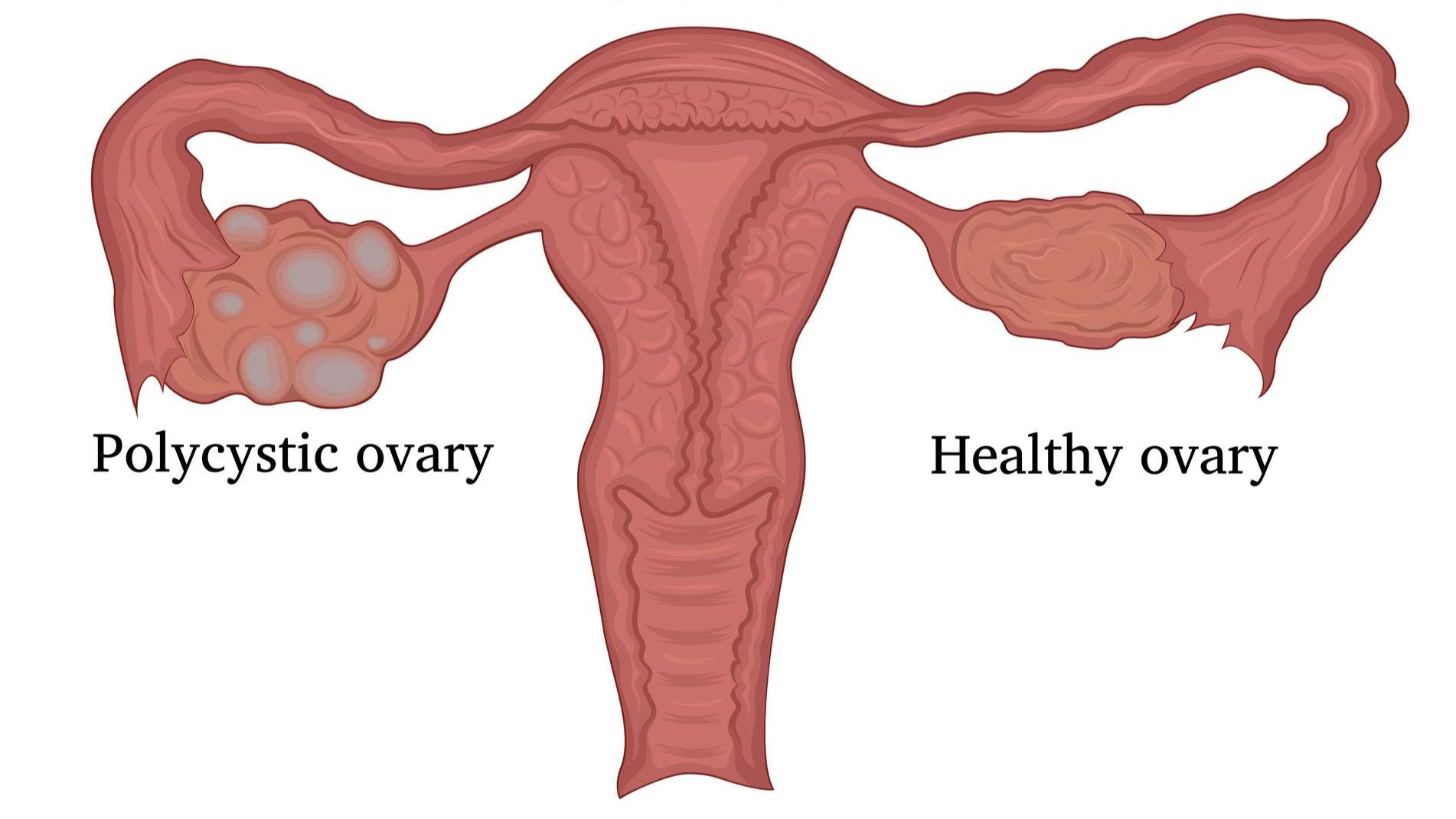
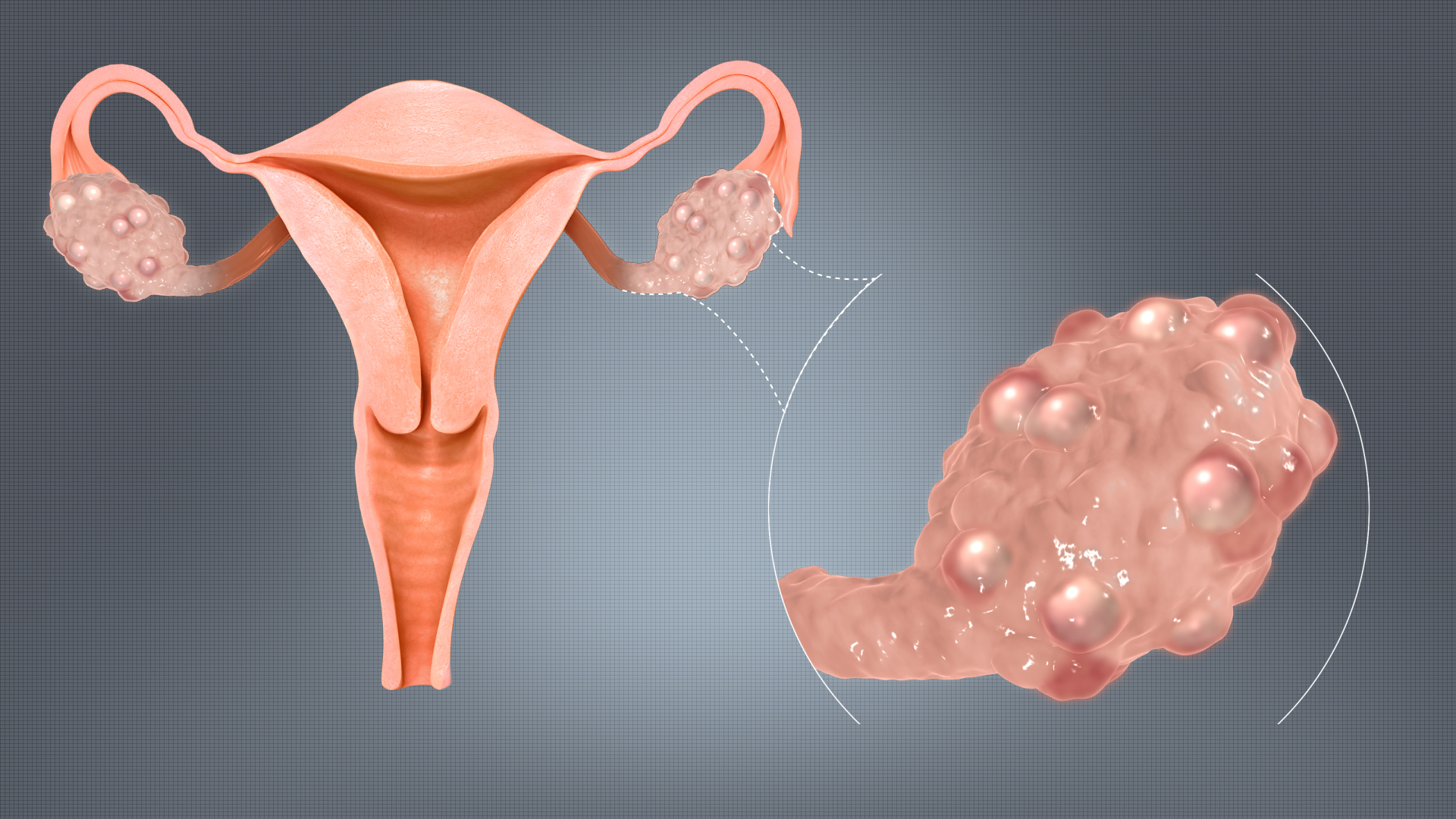
Polycystic Ovarian Disease (PCOD) is a condition where the ovaries produce multiple immature follicles often referred to as cysts that can interfere with normal ovulation. Like PCOS, it involves hormonal imbalances and irregular periods, but PCOD is generally considered less severe and more influenced by lifestyle factors.
The term PCOD is more commonly used in countries like India and some parts of Asia, and while it shares similarities with PCOS, it’s not always recognized globally as a distinct medical diagnosis. In many cases, PCOD is seen as a milder or earlier stage of what could develop into PCOS if not addressed.
Key Characteristics of PCOD
- Ovarian Cysts: The ovaries may have multiple underdeveloped follicles that fail to release eggs regularly, but without the widespread hormonal disruptions seen in PCOS.
- Milder Symptoms: Individuals with PCOD may still experience symptoms like irregular periods or mild acne, but they’re often less intense compared to PCOS.
- Lifestyle-Driven: PCOD is more commonly linked to poor diet, lack of exercise, high stress, and weight fluctuations. In many cases, lifestyle changes alone can significantly reduce or reverse symptoms.
Where PCOD and PCOS Overlap
- Both conditions may involve insulin resistance, irregular ovulation, and fertility challenges.
- Symptoms like weight gain, acne, and hair growth can occur in both, but their intensity and underlying hormonal patterns may differ.
- Because there’s no universal diagnostic criteria for PCOD, and the terms are often used interchangeably, many people may be diagnosed based on regional medical practices rather than standardized definitions.
Understanding the subtle differences between PCOS and PCOD is important, as it influences how doctors assess risk factors and design treatment plans especially when it comes to long-term health and fertility goals.
PCOS vs PCOD: What Sets Them Apart?
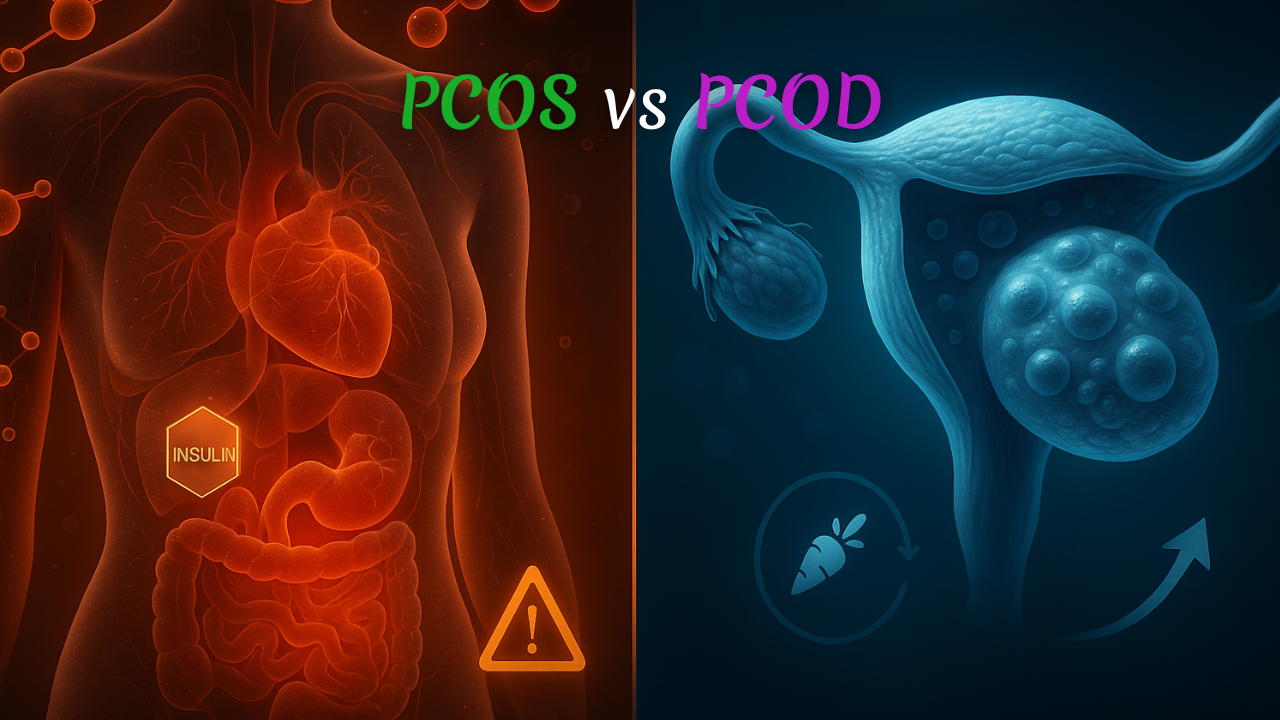
While PCOS and PCOD share many overlapping symptoms, they are not the same condition. The differences lie in their severity, causes, long-term impact, and how they respond to treatment. Understanding these distinctions can help guide more personalized care and improve health outcomes.
1. Hormonal Imbalance and Systemic Impact
- PCOS is often marked by more severe hormonal disruption especially elevated androgen (male hormone) levels and insulin resistance. These imbalances can affect multiple systems in the body, from the skin to metabolism to reproductive function.
- PCOD, on the other hand, may involve milder hormonal fluctuations. The changes are often more localized to the ovaries and may not impact the body as systemically as PCOS does.
2. Risk of Long-Term Health Complications
- PCOS carries a higher risk of developing chronic health issues such as type 2 diabetes, metabolic syndrome, high blood pressure, endometrial hyperplasia, and persistent fertility problems.
- PCOD also requires attention, but if managed early especially with lifestyle changes—the long-term risks are usually lower and more manageable.
3. Possibility of Reversal
- PCOS is generally considered a lifelong condition that needs consistent medical and lifestyle management. While symptoms can improve and even go into remission, complete reversal is uncommon without sustained effort.
- PCOD is often more responsive to lifestyle changes. Improvements in diet, physical activity, and stress management can sometimes restore normal ovarian function and menstrual regularity.
4. Diagnosis and Medical Classification
- PCOS is a formally recognized medical syndrome with international diagnostic criteria, such as the Rotterdam criteria, used by healthcare professionals worldwide.
- PCOD is more of a region-specific term, especially prevalent in countries like India. It doesn’t have universally accepted diagnostic guidelines and is sometimes considered a less severe or earlier form of PCOS.
Recognizing these key differences empowers individuals to make informed decisions about their health and allows healthcare providers to tailor treatment strategies accordingly. Whether you’re managing symptoms or exploring a diagnosis, understanding how PCOS and PCOD differ is a critical step toward effective care.
The Hormonal Imbalance Behind PCOS and PCOD

Hormones act like the body’s internal messaging system regulating everything from the menstrual cycle and metabolism to skin health and mood. In conditions like PCOS and PCOD, this messaging gets disrupted, throwing multiple systems out of balance.
Let’s break down how specific hormones contribute to the symptoms and complications seen in these conditions.
1. Androgens (Male Hormones)
People with PCOS or PCOD often have higher-than-normal levels of androgens such as:
- Testosterone
- DHEAS (Dehydroepiandrosterone sulfate)
- Androstenedione
When these hormones rise, they can lead to symptoms like:
- Acne and oily skin
- Excess facial or body hair (hirsutism)
- Thinning hair on the scalp (androgenic alopecia)
These outward signs are often among the first clues that hormonal levels are out of sync.
2. Estrogen and Progesterone
During a normal menstrual cycle:
- Estrogen helps build the uterine lining.
- Progesterone, released after ovulation, stabilizes this lining and prepares the body for pregnancy.
But in PCOS or PCOD, irregular or absent ovulation means progesterone stays low, while estrogen continues to build up. This imbalance can lead to:
- Irregular or heavy periods
- Increased risk of endometrial hyperplasia, a thickening of the uterine lining that can cause complications over time.
3. Insulin
Many people with PCOS or PCOD have insulin resistance, where cells don’t respond properly to insulin, the hormone that regulates blood sugar. In response, the body produces more insulin, which can:
- Stimulate the ovaries to produce even more androgens
- Worsen symptoms like weight gain, cravings, and fatigue
- Increase long-term risks like type 2 diabetes and metabolic syndrome
This hormonal domino effect shows just how interconnected the body’s systems are and why managing PCOS and PCOD often requires a comprehensive, hormone-focused approach that goes beyond just treating surface symptoms.
What Causes PCOS and PCOD? Understanding the Risk Factors
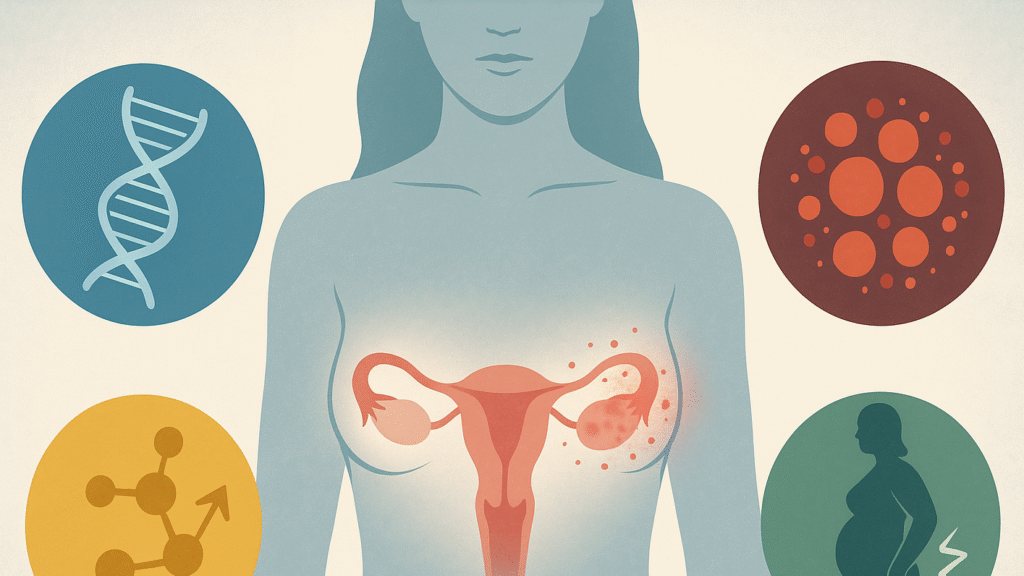
The exact cause of PCOS and PCOD isn’t fully understood, but research shows that both conditions result from a complex interaction between genetics, metabolism, hormones, and lifestyle. Some people may be more biologically prone to developing them, while others may see symptoms triggered or worsened by daily habits.
Let’s break down the key contributors:
1. Genetic Predisposition
- If you have a close family member—like a mother or sister—with PCOS or PCOD, your risk is significantly higher.
- Studies have identified certain genetic markers linked to insulin resistance and elevated androgens (male hormones), both of which are core features of these conditions.
- However, having the genes doesn’t guarantee you’ll develop symptoms—lifestyle factors often determine how those genes express.
2. Insulin Resistance
- This is one of the most common underlying issues in both PCOS and PCOD.
- When the body becomes less sensitive to insulin, the pancreas produces more to keep blood sugar in check.
- Excess insulin can trigger the ovaries to produce more androgens, disrupting ovulation and menstrual cycles.
- Over time, this feedback loop can lead to weight gain, irregular periods, and fertility problems.
3. Chronic Inflammation
- Many individuals with PCOS or PCOD show signs of low-grade, chronic inflammation—an internal state that worsens insulin resistance and affects ovarian health.
- Inflammatory markers like C-reactive protein (CRP) are often elevated.
- Diets high in refined sugars, processed foods, and unhealthy fats can amplify this inflammatory state.
4. Lifestyle and Environmental Factors
- Obesity: Excess body fat, especially around the abdomen, makes insulin resistance worse and increases hormonal imbalance.
- Physical inactivity: A sedentary lifestyle reduces insulin sensitivity, increasing the risk of metabolic dysfunction.
- Chronic stress: Long-term stress can disrupt the hypothalamic-pituitary-ovarian (HPO) axis, a hormonal feedback loop essential for reproductive health. Stress also increases cortisol, which may further raise insulin and androgen levels.
In most cases, it’s not just one factor but a combination of genetics, hormones, and lifestyle that drives the development and progression of PCOS and PCOD. That’s why a holistic, personalized approach to management is so important.
Recognizing the Signs and Symptoms of PCOS and PCOD

Symptoms of PCOS and PCOD can show up in many different ways, and no two people experience them exactly the same. Some may have only mild symptoms, while others face more pronounced changes that affect daily life. Understanding the most common signs can help you spot issues early and seek timely support.
1. Menstrual Irregularities
Hormonal imbalances often disrupt the menstrual cycle:
- Irregular periods: Menstrual cycles may become infrequent (known as oligomenorrhea) or stop altogether (amenorrhea).
- Heavy or prolonged bleeding: When ovulation doesn’t occur regularly, the uterine lining can build up for too long, leading to heavier periods when bleeding finally begins.
2. High Androgen (Male Hormone) Symptoms
Elevated androgen levels are a key feature of both PCOS and PCOD:
- Acne and oily skin: Increased oil production can cause persistent breakouts, especially around the jawline and chin.
- Hirsutism: Excess facial and body hair growth commonly on the upper lip, chin, chest, or back.
- Hair thinning or hair loss: Often seen on the scalp, this is called androgenic alopecia and resembles male-pattern baldness.
3. Weight Challenges and Metabolic Signs
Metabolism can slow down, making weight management more difficult:
- Unexplained weight gain, especially around the belly (central obesity), is common.
- Difficulty losing weight: Standard diet and exercise plans may not be as effective unless insulin resistance and hormone levels are addressed directly.
4. Emotional and Mental Health Effects
Hormonal shifts affect more than just the body—they can impact mood and mental well-being:
- Mood swings and irritability may become more noticeable.
- Anxiety and depression are more common in those living with PCOS or PCOD, influenced by both biological and emotional factors—including body image, fertility concerns, and chronic symptoms.
While symptoms can vary widely in intensity and combination, being aware of these hallmark signs is key to early diagnosis and effective treatment. If you recognize several of these in yourself or a loved one, it’s worth having a conversation with a healthcare provider.
How PCOS and PCOD Are Diagnosed: Tests and Medical Evaluation
Getting an accurate diagnosis of PCOS or PCOD requires more than a single test. Healthcare providers typically use a combination of symptom assessment, hormone testing, and imaging to confirm the condition and rule out other possible causes. Early diagnosis is crucial it allows for personalized treatment and helps prevent long-term complications like infertility, diabetes, or heart disease.
1. Pelvic Ultrasound
- Transvaginal ultrasound is commonly used to get a clear view of the ovaries and uterus.
- It helps detect the presence of multiple small follicles (cysts) and assess ovarian size.
- The scan can also measure endometrial thickness, which gives insight into how the menstrual cycle is functioning.
2. Blood Tests
A comprehensive blood panel helps evaluate hormone levels and metabolic health:
- Hormonal markers: Levels of LH (Luteinizing Hormone), FSH (Follicle-Stimulating Hormone), testosterone, DHEAS, and prolactin are assessed to identify imbalances.
- Blood sugar and insulin: Fasting glucose and insulin tests can detect insulin resistance, a key driver of PCOS and often present in PCOD.
- Lipid profile: High cholesterol or triglycerides may point to metabolic syndrome, which frequently coexists with PCOS.
3. Physical Examination
A basic clinical exam can also provide important clues:
- Vital signs: Blood pressure and Body Mass Index (BMI) are measured to assess metabolic risk.
- Visible symptoms: Doctors may look for signs like excess facial/body hair, acne, or acanthosis nigricans (dark, velvety skin patches, often linked to insulin resistance).
4. Medical and Menstrual History
Your doctor will ask detailed questions to piece together your health timeline:
- Menstrual patterns: Are your periods regular, heavy, or frequently missed?
- Family history: A background of PCOS, diabetes, or hormonal disorders in close relatives can raise suspicion.
- Other symptoms: Information about weight changes, mood shifts, and fertility attempts can help form a complete picture.
Doctors often use the Rotterdam criteria to diagnose PCOS, which requires at least two out of three findings:
- Irregular or absent ovulation
- Elevated androgen levels (clinically or in bloodwork)
- Polycystic ovaries visible on ultrasound
For PCOD, diagnosis tends to be more region-specific and less standardized, often based on a combination of ultrasound results and clinical symptoms.
Long-Term Health Risks of PCOS and PCOD: What You Should Know

If left unmanaged, both PCOS and PCOD can lead to a variety of long-term health complications. These aren’t just limited to reproductive issues—hormonal imbalances can ripple across your entire body, affecting your metabolism, heart, and mental well-being. That’s why early diagnosis and consistent management are so important.
1. Infertility and Ovulation Issues
- Irregular or absent ovulation (anovulation) can make it difficult to conceive naturally.
- While fertility challenges are common, they’re not always permanent. Medications like clomiphene citrate or letrozole can often help induce ovulation in people trying to get pregnant.
- With the right medical support, many individuals with PCOS or PCOD go on to have healthy pregnancies.
2. Metabolic Syndrome and Blood Sugar Imbalance
- Metabolic syndrome is a group of risk factors that raise your chances of developing chronic illnesses. It includes:
- Obesity (especially belly fat)
- High blood pressure
- Elevated blood sugar
- Abnormal cholesterol levels
- Because insulin resistance is common in both PCOS and PCOD, these individuals are at a higher risk for type 2 diabetes, fatty liver, and other metabolic complications.
3. Heart and Vascular Health
- High blood pressure (hypertension) can develop over time due to persistent insulin resistance and inflammation.
- Atherosclerosis, or the hardening of arteries, can occur when bad cholesterol (LDL) levels are high and good cholesterol (HDL) is low.
- Together, these factors significantly increase the risk of heart disease and stroke, especially as one gets older.
4. Emotional and Mental Health Concerns
- Living with PCOS or PCOD can be emotionally draining. Hormonal imbalances themselves may contribute to depression, mood swings, and low motivation.
- Anxiety, especially around fertility, body image, or weight, is common—and often underdiagnosed.
- Support from healthcare professionals, counselors, and peer groups can make a meaningful difference in managing mental health alongside physical symptoms.
With proper treatment whether through medications, hormone regulation, diet, exercise, or stress management many of these risks can be reduced or even prevented. Taking action early and maintaining a long-term plan is key to protecting your health and quality of life.
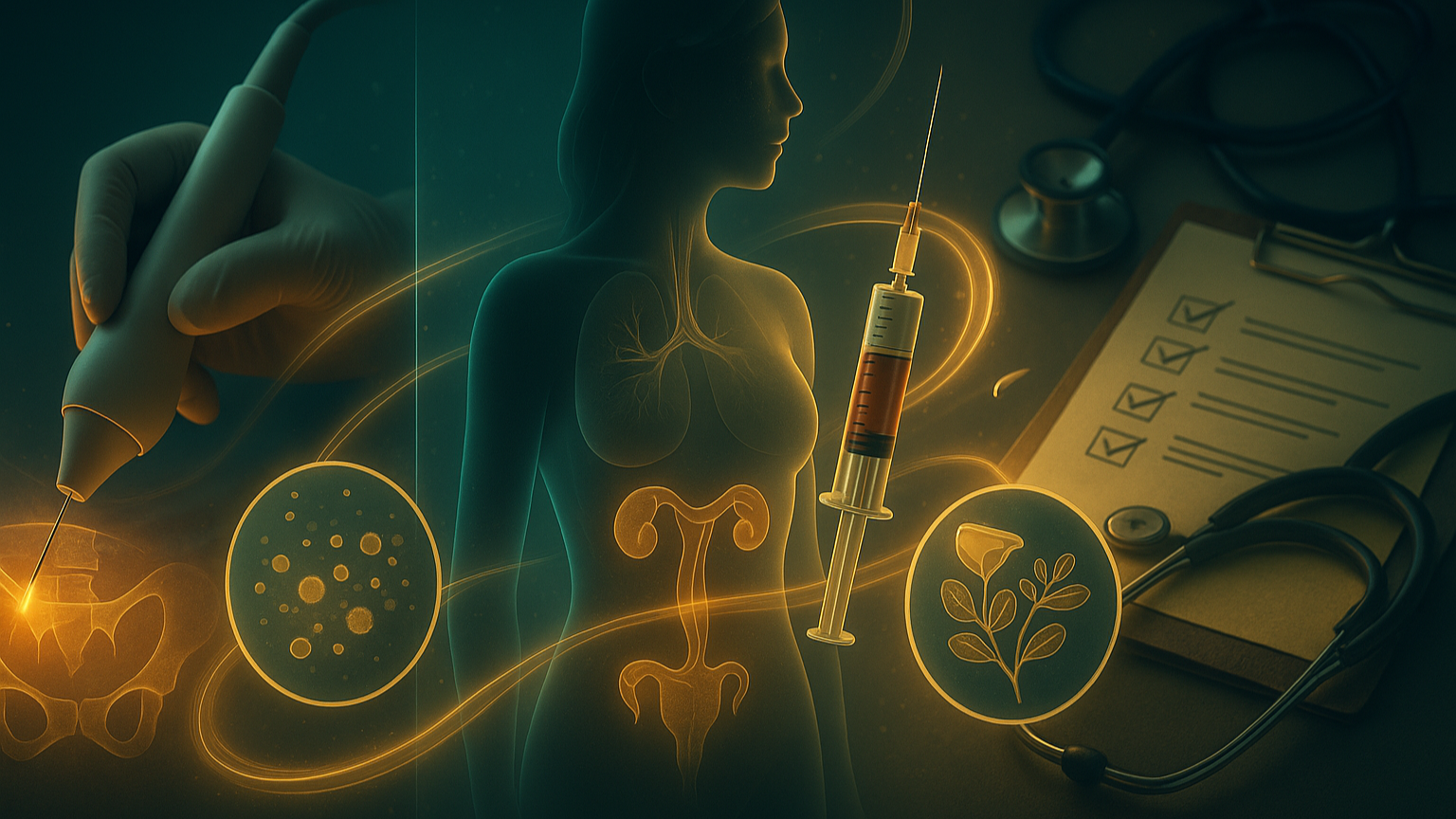
Effective Treatments and Therapies for PCOS and PCOD
Managing PCOS or PCOD effectively requires a personalized, multi-layered approach. No single solution works for everyone, but the right combination of lifestyle changes, medical treatments, nutrition, and holistic therapies can help restore hormonal balance, support reproductive health, and reduce long-term risks.
1. Lifestyle Modifications: The First Line of Defense

Weight Management
Losing even 5–10% of your total body weight can significantly improve hormonal balance, regulate menstrual cycles, and enhance fertility especially if insulin resistance is present.
Balanced Diet
A diet rich in whole, unprocessed foods helps manage insulin, reduce inflammation, and support long-term health.
- What to include:
- Whole grains: oats, brown rice, quinoa
- Lean proteins: eggs, chicken, tofu, legumes
- Healthy fats: avocados, olive oil, nuts, seeds
- Fiber-rich foods: leafy greens, berries, lentils
- What to limit or avoid:
- Sugary snacks and drinks
- White bread, pastries, and high-glycemic foods
- Trans fats found in fried or heavily processed foods
Sample Daily Meal Plan
- Breakfast: Oatmeal topped with berries and nut butter
- Snack: Apple with almonds
- Lunch: Grilled chicken salad with olive oil dressing
- Snack: Carrot sticks and hummus
- Dinner: Salmon with roasted vegetables and quinoa
- Optional Evening Snack: Greek yogurt or a piece of dark chocolate
2. Medications for Symptom Control and Hormonal Support

Metformin
Originally used for type 2 diabetes, metformin improves insulin sensitivity and can help regulate ovulation and reduce androgen levels.
Anti-Androgen Medications
Drugs like spironolactone are often prescribed to reduce acne, hair growth (hirsutism), and scalp hair thinning by blocking excess androgens.
Hormonal Contraceptives
- Combined oral contraceptive pills (estrogen + progesterone) help regulate menstrual cycles, reduce acne, and lower androgen levels.
- Progestin-only pills may be an option for those who cannot take estrogen but are less commonly used for PCOS.
3. Fertility Treatments

For individuals facing infertility due to irregular or absent ovulation:
- Ovulation induction with medications like clomiphene citrate or letrozole can stimulate egg release.
- In Vitro Fertilization (IVF) may be recommended if simpler treatments are unsuccessful.
4. Exercise and Movement

Benefits of Physical Activity
- Improves insulin sensitivity
- Lowers androgen levels
- Supports sustainable weight management
- Boosts mood through endorphin release
Best Types of Exercise
- Cardio (aerobic): brisk walking, cycling, swimming
- Strength training: resistance bands, weightlifting, bodyweight exercises
- HIIT (High-Intensity Interval Training): short bursts of effort followed by rest—excellent for metabolism
Tips for Getting Started
- Start with 10 minutes/day and build up
- Choose activities you enjoy to stay consistent
- Stay hydrated and listen to your body
5. Mental and Emotional Wellness

Hormonal imbalances don’t just affect the body they also impact mental health. Addressing emotional well-being is an essential part of managing PCOS/PCOD.
Stress Reduction
- Elevated cortisol (stress hormone) can worsen insulin resistance and disrupt the hormonal axis.
- Practices like deep breathing, journaling, or creative hobbies help regulate stress responses.
Therapy and Support
- Cognitive Behavioral Therapy (CBT) can help with anxiety, depression, or emotional eating.
- Peer support groups, whether local or online, can reduce feelings of isolation and provide motivation.
Mindfulness and Meditation
- Mindful eating improves your relationship with food and may help reduce binge episodes.
- Meditation or guided relaxation supports emotional balance and may reduce cortisol levels over time.
6. Herbal and Natural Remedies
In addition to conventional treatments, many individuals with PCOS or PCOD turn to natural remedies to support hormone regulation, ease symptoms, and improve overall wellness. While these options should not replace medical care, they can serve as powerful complementary tools when used thoughtfully and under professional guidance.
Natural remedies work best as part of a holistic lifestyle approach one that includes a healthy diet, regular movement, and stress management. Below are some of the most widely researched and commonly used herbs, adaptogens, and functional mushrooms for PCOS and PCOD support:
🌿 Ashwagandha (Withania somnifera)

A powerful adaptogenic herb in Ayurvedic medicine, ashwagandha is known for its ability to calm the nervous system and rebalance stress hormones.
- Supports cortisol reduction, helping the body respond better to chronic stress
- Improves adrenal function, essential for stabilizing overall hormone output
- May help lower testosterone in women with elevated levels
- Can promote better sleep, emotional balance, and reduce symptoms of anxiety and depression
🧠 Ideal for: Stress-related hormonal disruption, mood instability, adrenal fatigue, and insomnia
🌿 Cinnamon (Cinnamomum verum)

More than just a spice, cinnamon has been shown to have insulin-sensitizing effects, making it beneficial for metabolic support.
- Enhances glucose uptake and insulin efficiency
- Helps lower fasting blood sugar levels
- May support menstrual cycle regulation through improved insulin sensitivity
🍽 How to use: Sprinkle into smoothies, oats, or tea; or take as a supplement (Ceylon cinnamon is preferred for safety)
🌿 Spearmint

This refreshing herb has gained popularity for its anti-androgenic properties.
- Regular consumption of spearmint tea has been shown to reduce testosterone levels
- May help reduce hirsutism (facial/body hair growth)
- Can improve skin health and lessen hormonal acne
🍵 Recommended: 1–2 cups of spearmint tea daily for 1–2 months
🌿 Fenugreek (Trigonella foenum-graecum)

Often used in seed or supplement form, fenugreek is recognized for its hormone-balancing effects.
- Enhances insulin sensitivity
- May promote healthy estrogen and progesterone levels
- Can help restore ovulation and improve menstrual regularity
- Also beneficial for breast milk production in nursing mothers
🛑 Note: Use with caution if trying to conceive, as it may influence hormone levels
💊 Myo-Inositol & D-Chiro-Inositol

These natural compounds (vitamin-like substances) are commonly used in clinical PCOS protocols.
- Improve ovarian function and promote regular ovulation
- Reduce insulin resistance and testosterone levels
- May enhance egg quality and fertility outcomes
- Often used as a first-line supplement before fertility drugs
💡 Best taken in a 40:1 myo- to d-chiro-inositol ratio for optimal effect
Medicinal mushrooms are gaining attention for their adaptogenic, anti-inflammatory, and endocrine-supportive effects. Here are three functional mushrooms for PCOS/PCOD
🍄 Reishi Mushroom (Ganoderma lucidum)

Known as the “queen of mushrooms,” reishi is a calming adaptogen with broad health benefits.
- Helps lower elevated testosterone
- Supports immune balance and reduces chronic inflammation
- Calms the nervous system and supports better sleep
- May assist with stress-induced hormonal fluctuations
💤 Great for: Individuals with anxiety, insomnia, or inflammation-related PCOS
🍄 Cordyceps

Cordyceps are known for their energy-enhancing and metabolism-supportive effects.
- Boosts cellular energy (ATP), making it easier to stay active
- Improves endurance, helpful for maintaining a regular exercise routine
- Supports adrenal function, helping regulate fatigue and burnout
⚡ Best for: Those experiencing fatigue, low motivation, or adrenal dysfunction
🍄 Lion’s Mane (Hericium erinaceus)

While primarily known for brain health, Lion’s Mane also supports mental clarity and emotional regulation critical areas for those managing chronic hormonal conditions.
- Enhances neurogenesis and cognitive function
- May reduce anxiety and depression
- Supports nerve repair and gut-brain connection—often affected in PCOS
🧠 Useful for: Brain fog, mood swings, emotional burnout
✅ Important Note: Always speak with a qualified healthcare provider before starting any new supplement especially if you’re on medication, pregnant, breastfeeding, or undergoing fertility treatments. Some herbs can interact with pharmaceuticals or affect hormone-sensitive conditions.
While herbal and mushroom-based therapies won’t cure PCOS or PCOD on their own, they can become invaluable allies in a broader treatment plan especially when personalized to your specific hormonal needs.
Combined with proper nutrition, medical support, stress reduction, and movement, these natural tools may offer not only symptom relief but also a more balanced, resilient body and mind.
7. Complementary Therapies

Ayurveda
- A traditional system that uses customized herbal remedies, detoxification, and diet adjustments
- Common herbs: Shatavari, Tulsi, Guggul, and Brahmi
Acupuncture
- May help regulate gonadotropin levels and improve insulin sensitivity
- Also used to reduce stress and support menstrual regularity
Yoga
- Combines physical movement, breathwork, and mindfulness
- Reduces cortisol, improves flexibility, and supports emotional balance ideal for those with limited mobility
Final Word on Treatment Strategy
The most effective PCOS or PCOD treatment plans are tailored to the individual taking into account your symptoms, goals (like fertility), and long-term health needs. Combining medical therapies, lifestyle upgrades, and natural support offers the best chance of managing symptoms and improving overall well-being.
Frequently Asked Questions (FAQs) About PCOS and PCOD
These are some of the most commonly searched and asked questions about PCOS (Polycystic Ovary Syndrome) and PCOD (Polycystic Ovarian Disease) answered clearly to help you make informed decisions about your health.
1. Can PCOS or PCOD be cured permanently?
Searches: Is there a permanent cure for PCOS? | How to cure PCOD naturally?
There’s currently no guaranteed “permanent cure” for PCOS or PCOD. However, many people experience long-term symptom relief—or even remission—by consistently managing their lifestyle, following medical guidance, and addressing hormonal imbalances. Key areas to focus on include diet, exercise, stress reduction, and hormonal therapy when needed.
2. What is the difference between PCOS and PCOD?
Searches: Are PCOS and PCOD the same? | PCOD vs PCOS difference
While the terms are often used interchangeably, they aren’t exactly the same:
- PCOS is a more complex hormonal syndrome, officially recognized with global diagnostic criteria and often involving insulin resistance, high androgens, and metabolic complications.
- PCOD refers to ovarian dysfunction with cyst formation, typically seen as a milder or more lifestyle-driven condition.
3. Can I get pregnant with PCOS or PCOD?
Searches: Can women with PCOS get pregnant naturally? | PCOD and fertility
Yes, many individuals with PCOS or PCOD do conceive naturally, especially with healthy lifestyle practices and menstrual regulation. For those who face challenges, fertility treatments like ovulation induction (using clomiphene or letrozole) or IVF can significantly improve the chances of pregnancy.
4. Is it safe to take birth control pills for PCOS or PCOD?
Searches: Best birth control for PCOS | Do birth control pills help PCOD?
Yes. Combined oral contraceptive pills are commonly prescribed to:
- Regulate periods
- Lower testosterone levels
- Reduce acne and unwanted hair growth
However, your doctor will help choose the safest option based on your health profile, goals (e.g., fertility), and potential side effects.
5. What foods should I eat or avoid with PCOS/PCOD?
Searches: Best diet for PCOS | Foods to avoid in PCOD
A balanced, low-glycemic diet is highly recommended. Focus on:
- What to eat: leafy greens, berries, legumes, lean proteins, healthy fats, whole grains
- What to avoid: refined carbs (white bread, sugary snacks), fried foods, sugary beverages
These changes can significantly improve insulin sensitivity, stabilize hormones, and support weight management.
6. Does stress make PCOS or PCOD worse?
Searches: Does stress affect PCOS? | How to reduce stress for hormonal balance
Yes. Chronic stress elevates cortisol, which can interfere with your body’s ability to regulate insulin and sex hormones worsening symptoms like irregular cycles, acne, and weight gain. Stress management techniques such as meditation, deep breathing, yoga, journaling, or therapy can be incredibly beneficial.
7. Can thin women have PCOS or PCOD?
Searches: PCOS without obesity | Is PCOS only for overweight women?
Absolutely. PCOS and PCOD affect people of all body types. In fact, a subset known as “lean PCOS” involves individuals who may not have visible weight issues but still struggle with hormonal imbalances, irregular periods, or infertility.
8. Is hair thinning or hair loss in PCOS/PCOD reversible?
Searches: How to reverse hair loss in PCOS? | Best treatment for PCOS hair thinning
Hair loss from elevated androgens (testosterone, DHEAS) may be partially reversible if addressed early. Treatments can include:
- Anti-androgen medications (like spironolactone)
- Topical minoxidil
- Diet and stress management
- Supplements such as zinc, iron, and biotin (as prescribed)
Consistency is key for seeing results.
9. Are natural remedies effective for PCOS or PCOD?
Searches: Herbal cure for PCOS | Natural treatment for PCOD
Natural remedies like herbal supplements (ashwagandha, spearmint, cinnamon), functional mushrooms, and inositol compounds can support hormone balance and symptom relief. However, they work best when combined with a healthy lifestyle and under a doctor’s guidance especially if you’re on medication or trying to conceive.
10. How often should I visit my doctor if I have PCOS or PCOD?
Searches: PCOS monitoring schedule | How often to check hormone levels
It depends on your individual case and treatment plan, but check-ups every 3 to 6 months are typical. During follow-ups, your doctor may monitor:
- Hormone levels
- Blood sugar and insulin
- Menstrual patterns
- Weight and blood pressure
- Medication side effects
Regular monitoring ensures timely adjustments and prevents complications.
Still Have Questions?
Leave a comment or consult a licensed healthcare professional to get personalized guidance. And don’t forget to visit our full guide above for in-depth information on symptoms, causes, and the latest treatment options.
Conclusion: Understanding PCOS and PCOD for Better Health Outcomes
PCOS (Polycystic Ovary Syndrome) and PCOD (Polycystic Ovarian Disease) are two of the most common hormonal conditions affecting people with ovaries—often misunderstood, underdiagnosed, or mistaken for one another. While both conditions share symptoms like irregular periods, acne, unwanted hair growth, and weight challenges, their root causes and long-term impacts can vary.
PCOS is typically more systemic and complex, involving hormonal and metabolic disruptions that can affect the ovaries, blood sugar regulation, and heart health. PCOD, while still serious, may be less intense and often more responsive to lifestyle changes like better nutrition, regular physical activity, and stress reduction.
Whether you’re newly diagnosed or just starting to ask questions like “Why is my period irregular?” or “How do I know if I have PCOS or PCOD?”, this guide offers the essential foundation to move forward with confidence.
Key Takeaways
- PCOS is an endocrine syndrome with broader hormonal disruption, often leading to chronic anovulation, insulin resistance, and higher androgen levels.
- PCOD involves the presence of multiple ovarian cysts but may show fewer systemic symptoms and respond more quickly to diet, exercise, and stress management.
- Common symptoms include:
- Irregular or missed periods
- Acne and oily skin
- Unwanted facial/body hair (hirsutism)
- Hair thinning on the scalp
- Weight gain, especially around the abdomen
- Anxiety, mood swings, or difficulty with fertility
- Causes are often a mix of genetics, insulin resistance, inflammation, and environmental factors (diet, stress, sedentary lifestyle).
- Best treatment approaches combine:
- Medical care: Metformin, anti-androgens, hormonal contraceptives
- Dietary changes: Low-glycemic, high-fiber whole foods
- Exercise: Aerobic movement, strength training, yoga
- Mental health support: Mindfulness, therapy, and stress relief techniques
- Natural supplements: Ashwagandha, spearmint, inositol, and medicinal mushrooms (under medical guidance)
Why Early Action Matters
People often ask:
- “Can PCOS/PCOD go away on its own?”
- “Is it possible to reverse PCOS with diet and exercise?”
- “Can I live a normal life with PCOS?”
The truth is: early detection and consistent management are key. While there is no one-size-fits-all cure, many individuals go on to live full, healthy lives by taking charge of their hormonal health through informed decisions, sustainable habits, and regular medical check-ups.
Next Steps: Take Control of Your Hormonal Health
If you’re dealing with symptoms or even just suspect something’s off don’t ignore the signs. Speak with a qualified healthcare provider for personalized testing and a treatment plan tailored to your unique goals whether it’s fertility, clearer skin, regular periods, or simply feeling more energized and in control of your body.
Bonus tip: You can also use AI tools like ChatGPT to get a clearer idea of what might be going on before your doctor’s visit.
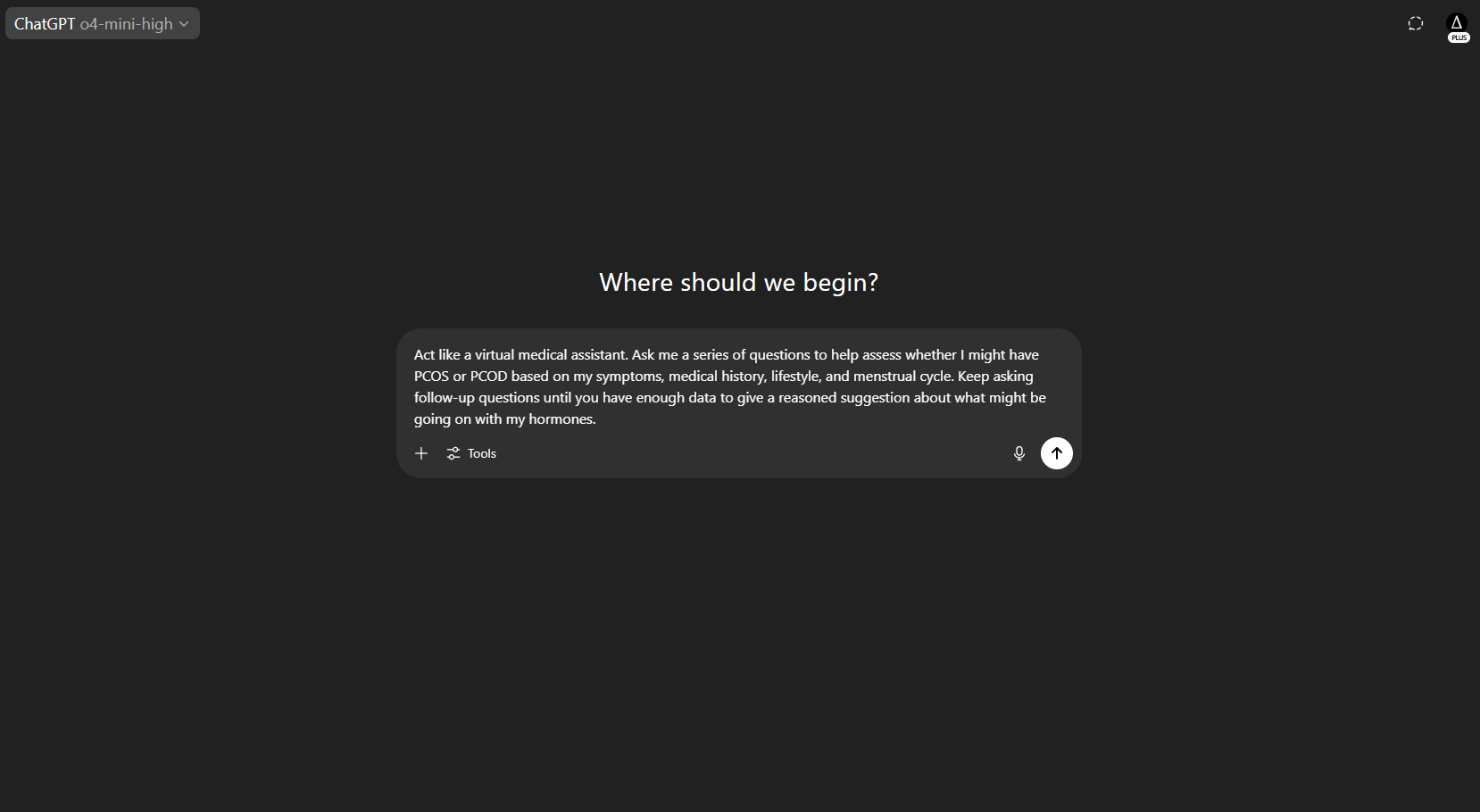
By using ChatGPT’s reasoning capabilities, you can work through a guided questionnaire that mimics an early clinical assessment. While this is not a replacement for medical diagnosis, it can help you understand your risk level and prepare smarter questions for your doctor.
Self-Check Prompt for PCOS or PCOD Risk (Copy & Paste into ChatGPT):
“Act like a virtual medical assistant. Ask me a series of questions to help assess whether I might have PCOS or PCOD based on my symptoms, medical history, lifestyle, and menstrual cycle. Keep asking follow-up questions until you have enough data to give a reasoned suggestion about what might be going on with my hormones.”
This interactive method can help you organize your thoughts, recognize patterns in your symptoms, and feel more confident when seeking care.
Stay Informed and Empowered
For more practical tips, science-backed insights, and supportive tools:
👉 Follow us on Instagram and other social media platforms for daily content
👉 Share this guide with friends or family who might benefit
👉 Bookmark this article so you can return to it anytime
Because understanding your body is the first step toward healing it—and you’re never alone on this journey.